All published articles of this journal are available on ScienceDirect.
Health Complaints Attributed to Dental Amalgam: A Retrospective Survey Exploring Perceived Health Changes Related to Amalgam Removal
Abstract
Background:
Many patients have complex health complaints they attribute to dental amalgam. There is some evidence of symptom relief after removal of amalgam.
Objective:
The aims of this study were to assess the total symptom load in patients with all their amalgam fillings removed, and to investigate the self-reported improvement of health with regard to precautions taken under amalgam removal and time since removal.
Methods:
The survey was distributed to all members (n=999) of the Norwegian Dental patients association in 2011. The study participants returned the questionnaires anonymously by means of a pre-stamped envelope. The questionnaire asked for sociodemographic data, subjectively perceived health status, complaints persisting after amalgam removal and self-reported changes in symptoms after amalgam removal.
Results:
A total of 324 participants were included in the study. The majority of the participants reported improved health after amalgam removal, even though the mean degree of severity of complaints was still high. Exhaustion and musculoskeletal complaints were most severe, and reflects the fact that 38% of the participants reported poor to very poor current health. With regard to amalgam removal, associations between improved health, number of precautions applied, and time since removal were found.
Conclusion:
Most of the participants in this study reported improvement of health after amalgam removal even though they still suffered a high complaint load. Since absolute symptom load is a robust predictor for general health outcome and socioeconomic burden for society, a possible intervention, which enables patients to further improve their health status is desirable.
INTRODUCTION
Many patients present to their General Practitioner (GP) with a high symptom load and considerable psychological distress. Often, the underlying pathophysiology remains unclear and sometimes these patients receive a diagnosis such as irritable bowel syndrome, chronic fatigue syndrome or fibromyalgia. Common to all these diagnoses is that their pathophysiology remains unclear and therefore often called “functional”. Patients do not die from these syndromes, but they suffer. Often they feel stigmatized and that their suffering is not accepted [1]. Moreover, the associated direct and indirect socioeconomic costs are substantial [2].
A number of different symptoms have been attributed to dental amalgam [3]. Although often transient, a sizeable proportion is persistent and associated with a considerable reduction in these patients’ quality of life. The most commonly reported complaints attributed to dental amalgam are neurological symptoms such as fatigue and dizziness, mental symptoms such as concentration and memory disturbance, anxiety, irritability, restlessness and depression. Moreover, pain in muscle joints and pain in neck, shoulder, teeth, jaws, face and headache as well as gastrointestinal symptoms such as constipation, diarrhoea, bloating, mouth blisters, metallic taste, as well as increased susceptibility to infections, are also commonly reported [4-11]. Many patients who had their amalgam fillings removed experience less severe symptoms after removal [8, 12-15]. Best results (higher degree of symptom improvement, general improvement or recovery) were seen in patients who had all their amalgam fillings removed.
In Norway, amalgam removal procedures in patients with health complaints attributed to dental amalgam, are supposed to follow the recommendations given in National guidelines for assessment and treatment for suspected adverse effects from dental biomaterials [16]. These recommendations intend to minimise exposure to mercury and other heavy metals during the removal procedures. They consist of: a) removal of the whole amalgam filling in chunks without any pulverizing; b) application of water cooling during the procedure; c) use of a sharp drill; and d) use of protective equipment including rubber dam, suction at the tooth and appropriate ventilation of the treatment room [16, 17]. In addition to these guidelines, the Norwegian Dental Patient Association (NDPA), (Forbundet tenner og helse (FTH) in Norwegian) claims that it is important to combine the removal of amalgam fillings with additional preventive therapies [18]. NDPA recommends patients to take supplements such as selenium, zinc, vitamin C and E in order to improve immune system functioning before, during and after the removal of amalgam. Just before the removal, the intake of charcoal tablets and one unit of alcohol [17, 18] is recommended for further protection alongside several other additional therapies [19]. These recommendations are often based on extrapolations from laboratory experiments in animals (e.g. alcohol inhibits uptake of mercury vapour from the lung through inhibition of the catalase enzyme [20]) and anecdotal experiences. Systematic scientific evidence that these precautions are associated with improved health outcomes in humans is however, currently missing. One randomized trial found no difference in general health complaints in patients who replaced amalgam and used additional “detoxification therapy” compared to patients who removed amalgam and did not use such therapy [5].
The aims of the present study were to (1) assess the total symptom load in patients who have had all their amalgam fillings removed and (2) investigate the self-reported improvement of health with regard to precautions taken under amalgam removal and time since removal.
MATERIAL AND METHODOLOGY
Study Population
This study was a part of a larger research program on potential negative health effects of amalgam, commissioned by the Norwegian Directorate of Health to the National Research Center in Complementary and Alternative Medicine (NAFKAM) in Norway. Patient participation was a cornerstone of this project, so the questionnaire used in the present survey was developed in close cooperation with NDPA. One of the aims of this program was to develop a rehabilitation program for patients who have had all their amalgam fillings removed, but still experienced symptoms. A part of this intervention should be based on a survey exploring the target groups’ experiences with different types of interventions that were not part of the official healthcare system in Norway [21]. The Norwegian Data Inspectorate (NSD) has been notified about the study and the Regional Committee for Medical and Health Research Ethics (REK) has considered the study (REK reference 2011/1281) and decided that no ethic approval was needed due to full anonymity of the participants.
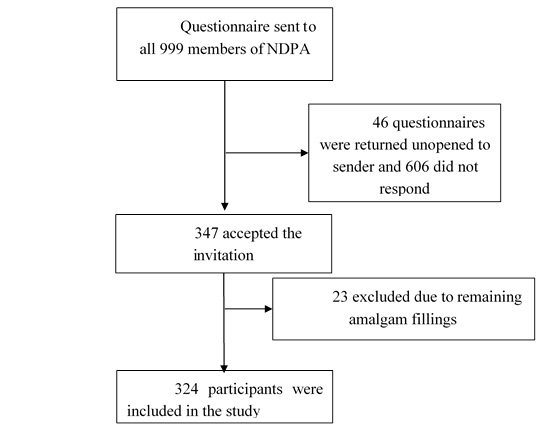
The survey was distributed through NDPA to all their members in December 2011. One reminder was sent in February 2012. The study participants returned the questionnaires anonymously to NAFKAM by means of a pre-stamped envelope. The questionnaire asked for sociodemographic data, subjectively perceived health status, complaints persisting after amalgam removal (based on Norwegian version of the Giessen Subjective Complaints List (GBB-24)), self-reported changes in symptoms after amalgam removal, and experience with different therapeutic interventions. The questionnaire also asked for use of complementary and alternative therapies, which are reported elsewhere [22]. The only criteria for inclusion were membership in the patient association NDPA and previously amalgam fillings of which all were removed. Since the target group of this survey were patients, who had their amalgam fillings removed, participants with remaining amalgam fillings were excluded from the analyses (n=23, Fig. 1). No information on possible medical diagnoses was obtained.
Health Complaints According to the GBB-24
The Giessen Subjective Complaints List (GBB-24) consists of 24 different health complaints. The severity of each complaint is rated according to a five point scale; 0 (not at all), 1 (slightly), 2 (somewhat), 3 (considerably) and 4 (very much) [23]. The complaints are grouped and summarized into four subscales with six complaints in each of the following groups: Cardiovascular complaints, gastrointestinal complaints, musculoskeletal complaints and exhaustion. Furthermore, the scores of the 24 single complaints are summed up in a total score (“complaints load”) ranging from 0-96 where 0 is no complaints at all while 96 represent all listed complaints at highest severity. In addition to the 24 items in the GBB-24 questionnaire, the participants were asked for severity of pain in the face and/or the jaw. This additional item was included because it reflects a symptom known to be relevant for the patient group studied (Table 2).
Since the average score for each item also includes participants answering “0” (not at all), it is difficult to estimate the severity of the health complaint in individuals suffering from the actual complaint. A low mean could reflect that many participants suffer this symptom, but not very intensely, or that only a few are affected, reporting a high intensity. Therefore, a second item analysis was performed, which included only data from participants answering 1 (slightly) or higher for a complaint. The reason for this was to explore the burden of each individual symptom among the individuals suffering the actual complaint.
Self-reported Changes in Health Following Amalgam Removal
Possible changes in self-reported health following the amalgam removal were addressed in two different questions:
For the main analyses, a general question with four response categories was used: “If you have replaced your amalgam fillings, do you consider your health to have changed as a consequence of this? 1. The health has improved, 2. The health has worsened, 3. The health is unchanged, 4. Don’t know.
In addition, another question addressed long-term changes with six response categories: “Have you experienced long-term (longer than 6 months) effects or changes following amalgam removal? 1. Worsening, 2. No change 3. Some improvement, 4. Major improvement 5. Total recovery / symptom free, 6. Don't know. The breakdown into six categories made this question less suitable for subgroup analysis, but still valuable for comparison to other studies with similar response categories.
Factors Perceived as Being Related to Amalgam Removal
Data on possible precautions made before, during and after the amalgam removal were collected via the following question:
If you have had dental fillings with amalgam removed, was there any precautions taken in connection with the replacement of fillings? (drugs / minerals / vitamins / protective equipment) Multiple answers possible. 1. Yes I had prophylactic treatment, 2. Yes, protective equipment was used during the dental treatment, 3. Yes, I had post treatment, 4. No, no precautions were made, 5. Don’t know.
Since this item allowed multiple answers, the analysis was performed according to the number of precautions (out of the responses 1, 2, 3 or 4 above) the participants reported: 0 (no precautions), 1 (one precaution), 2 (two precautions), 3 (three precautions). Table 3 includes a detailed analysis of the various combinations.
Statistics
Between-group differences were analysed using chi-square tests for binary data analysing one variable at the time, one-way ANOVA test for continuous data in SPSS for Windows (version 22.0, SPSS, Inc., Chicago, IL). Significance level was defined as p <0.05 without p-value adjustment for multiple comparisons.
RESULTS
Inclusion
A total of n=999 envelopes with questionnaires were sent out, of which 46 were returned unopened to sender. Overall, 953 members of NDPA received the questionnaire, 347 responded (36.4% response rate) and 324 fulfilled all eligibility criteria and were included in the study (Fig. 1).
Basic Characteristics of the Participants
The majority of the participants were female (71.6%), mean age was 60 years and 43.7% of the participants had university education. The women were slightly older than the men (2.5 years, p=0.001) and men were more often still working (p=0.014). Most participants reported normal (neither good nor poor) to good current health (62.4%) and improved health after amalgam removal (75.2%). However, a substantial number of participants reported poor to very poor current health (37.6%). No significant gender differences were found with regard to education or self-reported current health (Table 1). In order to avoid low cell frequencies, gender differences were not included in the further analysis.
| Total | Men | Women | p-value | |
|---|---|---|---|---|
| %(n) | %(n) | %(n) | ||
| Gender | ||||
| Women | 71.6 (232) | |||
| Men | 28.4 (92) | |||
| Age | ||||
| Mean | 60.0 | 58.8 (SD 11.12) | 61.3 (SD 10.26) | 0.001^ |
| Education | ||||
| Primary School | 13.4 (42) | 7.9 (7) | 15.6 (35) | 0.252* |
| Secondary School | 27.4 (86) | 32.6 (29) | 25.3 (57) | |
| High School | 15.6 (49) | 13.5 (12) | 16.4 (37) | |
| University, lower grade | 22.0 (69) | 25.8 (23) | 20.4 (46) | |
| University, higher grade | 21.7 (68) | 20.2 (18) | 22.2 (50) | |
| Working | ||||
| Yes | 59.0 (128) | 71.0 (49) | 53.4 (79) | 0.014* |
| No | 41.0 (89) | 29.0 (20) | 46.6 (69) | |
| Self-reported current health | 0.203* | |||
| Very good | 9.7 (31) | 15.4 (14) | 7.5 (17) | |
| Good | 25.4 (81) | 26.4 (24) | 25.0 (57) | |
| Neither good nor poor | 27.3 (87) | 23.1 (21) | 28.9 (66) | |
| Poor | 28.5 (91) | 28.6 (26) | 28.5 (65) | |
| Very poor | 9.1 (29) | 6.6 (6) | 10.1 (23) | |
| Changes in health after amalgam removal | 0.024* | |||
| Worsening of health | 8.4 (26) | 7.8 (7) | 8.6 (19) | |
| Unchanged health | 9.4 (29) | 4.4 (4) | 11.4 (25) | |
| Improved health | 75.2 (233) | 85.6 (77) | 70.9 (156) | |
| Don't know | 7.1 (22) | 2.2 (2) | 9.1 (20) | |
Health Complaints According to the GBB-24
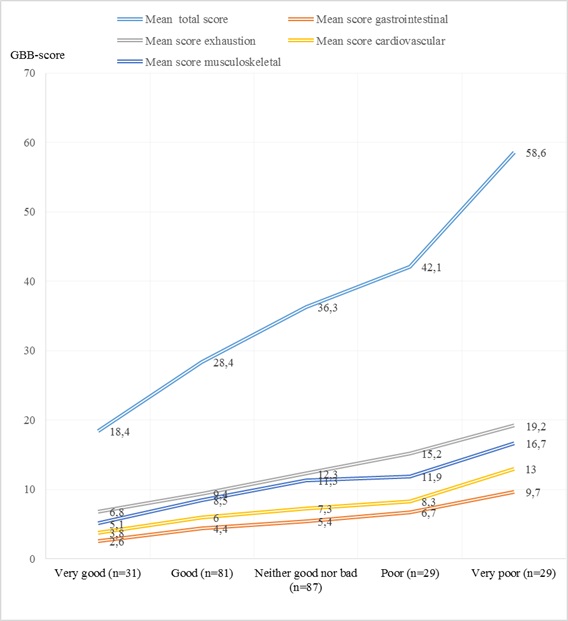
Mean severity score of the main 24 complaints in the GBB-24 (range 0-96) was 36.1 (47.8 in the group with less than one year since removal of amalgam, 39.6 one to four years, 35.0 five to nine years and 36.5 more than ten years after removal). Twenty-seven participants had a sum score of 0 (no complaints reported) while one participant reported highest possible degree of complain load, 96. The most commonly reported single symptoms among the participants were tendency of rapid exhaustion (80.9%) followed by tiredness (79.6%), concentration disturbances (77.5%) and pains in joints or limbs (75.6%). These four complaints were also the complaints with highest mean severity in the total sample (2.42, 2.18, 2.12 and 2.14 respectively, 2 indicating “somewhat” and 3 “considerable”). The mean severity of the remaining complaints were ranging from 0.42 (vomiting) to 2.00 (pain in neck and shoulders). When grouped into the following four subscales exhaustion, musculoskeletal complaints, cardiovascular complaints and gastrointestinal complaints (Table 2), we found that all symptom complexes were reported by more than 75% of the participants. When the intensity of the complaints were taken into consideration, exhaustion and musculoskeletal complaints were the most severe complaints with a mean severity score in the total sample of 12.46 and 10.65 respectively (Table 2). A considerably lower mean severity score in the total sample was found for cardiovascular and gastrointestinal complaints (7.34 and 5.65 respectively). The additional symptom Pain in the face or jaws was reported by 58.3% of the participants with a mean severity score in the total sample of 1.53 and a mean severity score among the participants actually suffering from the complaint of 2.62 (Table 2). As shown in Fig. (2), there was a linear correlation between symptom load and self-reported health in all groups of complaints, in particular for exhaustion and musculoskeletal complaints.
| Symptom/ GBB scale | % reporting | n | Mean severity in the total sample | Mean severity in participants reporting the symptom |
|---|---|---|---|---|
| TOTAL GBB-24 sum score | 91.70 | 297 | 36.10 | 58.41 |
| Exhaustion | 88.60 | 287 | 12.46 | 16.57 |
| Tendency to rapid exhaustion | 80.90 | 262 | 2.42 | 2.99 |
| Tiredness | 79.60 | 258 | 2.18 | 2.74 |
| Excessive need for sleep | 71.30 | 231 | 1.93 | 2.71 |
| Weariness | 71.30 | 231 | 1.91 | 2.68 |
| Physical weakness | 70.10 | 227 | 1.90 | 2.72 |
| Concentration disturbance * | 77.50 | 251 | 2.12 | 2.73 |
| Musculoskeletal complaints | 88.30 | 286 | 10.65 | 15.84 |
| Pains in joints and limbs | 75.60 | 245 | 2.14 | 2.83 |
| Backache | 65.40 | 212 | 1.71 | 2.61 |
| Headaches | 62.00 | 201 | 1.56 | 2.51 |
| Pains in neck and shoulders | 70.40 | 228 | 2.00 | 2.84 |
| Head pressure | 62.70 | 203 | 1.63 | 2.60 |
| Heaviness or tiredness in the legs | 66.40 | 215 | 1.62 | 2.45 |
| Cardiovascular complaints | 82.40 | 267 | 7.34 | 13.33 |
| Dizziness | 64.50 | 209 | 1.48 | 2.30 |
| Heavy, rapid or irregular heart-throbbing | 64.20 | 208 | 1.47 | 2.29 |
| Sudden bouts of heart-trouble | 48.50 | 157 | 1.03 | 2.13 |
| Twinges, pains or aching in the chest | 53.70 | 174 | 1.18 | 2.19 |
| Attacks of breathlessness | 48.80 | 158 | 1.06 | 2.16 |
| Sensation of tightness, choking or lumpiness in the throat | 49.70 | 161 | 1.12 | 2.26 |
| Gastrointestinal complaints | 76.50 | 248 | 5.65 | 12.67 |
| Stomach aches | 60.20 | 195 | 1.31 | 2.18 |
| Pressure or heaviness in the stomach | 51.20 | 166 | 1.17 | 2.28 |
| Heartburn | 46.60 | 151 | 1.04 | 2.24 |
| Nausea | 44.10 | 143 | 0.88 | 2.00 |
| Belching | 38.00 | 123 | 0.82 | 2.17 |
| Vomiting | 23.50 | 76 | 0.42 | 1.80 |
| Other, added to the GBB-24 complaints | ||||
| Pain in the face or jaws | 58.30 | 189 | 1.53 | 2.62 |
Factors, Perceived as Being Related to Amalgam Removal
Self-reported Changes in Health After Amalgam Removal
In response to the general question regarding changes in health after amalgam removal, the majority of the participants (75.2%, n=233) reported improvement of health, 8.4% (n=26) reported worsening of health while 9.4% (n=29) reported no change in health status. Seven percent (n=22) could not say whether their health has changed or not (Table 1). In a subgroup analysis according to current health, this was also the case in all subgroups except in the group reporting very poor health, in which more participants reported worsening of health (n=13) than improvement of health (n=11) after amalgam removal (Fig. 3).
In response to the additional question regarding long-term changes after amalgam removal, 8.6% (n=24) reported to be recovered / symptom free, 59.3% (n=166) reported major improvement, 17.5% (n=49) some improvement, 2.5% (n=7) no change, 8.9% (n=25) worsening, while 3.2% (n=9) responded “don't know”.
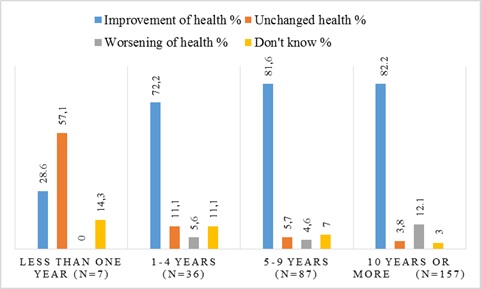
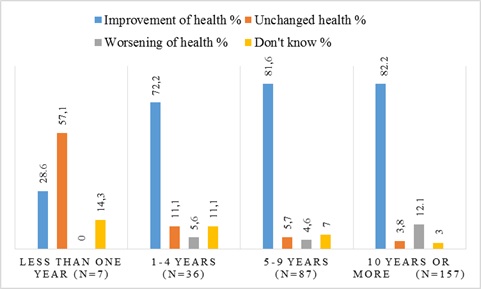
Experienced Changes in Health After Amalgam Removal Related to Time Since Removal
When the changes in health after amalgam removal (general question, see above) were analysed according to time since removal, we found that the highest number of participants reporting improved health after amalgam removal was found among the participants who have had their amalgam removed more than nine years ago (82.2%, n=129). The lowest report of improved self-reported health was found among the participants who had removed their amalgam within the last year (28.6%, n=2). Worsening of self-reported health after amalgam removal was highest (12.1%, n=19) in participants with more than 9 years since removal and lowest in the group who have had their amalgam removed within the last year (0.0%, n=0) (p<0.001, Fig. 4).
Experienced Changes in Health After Amalgam Removal Depending on the Conditions Related to the Removal
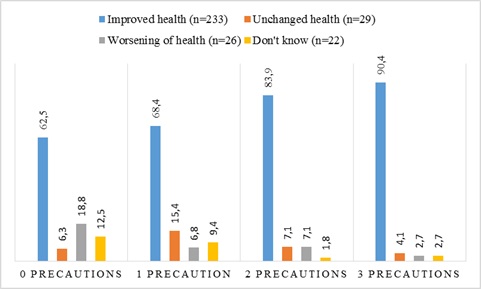
Among participants who had used no precautions neither before, during nor after the amalgam removal, 62.5% reported improved health, 6.3% reported no change and 18.8% reported worsening of health after removal. Among those who had used both prophylactic treatment, protective equipment and post-treatment, 90.4% reported improved health, 4.1% reported unchanged health, while 2.7% reported worsening of health after amalgam removal (p<0.001, (Fig. 5). The changes in health after amalgam removal for the different combination of precautions made are described in Table 3.
| Number of precautions | Combination of precautions | Improved health (n=233) | Unchanged health (n=29) | Worsening of health (n=26) | Don't know (n=22) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| 0 | No precautions | 40 | 60.6 | 4 | 6.1 | 12 | 18.2 | ||
| 1 | Only profilactic treatment | 11 | 78.6 | 1 | 7.1 | 1 | 7.1 | 1 | 7.1 |
| Only protective equipment | 62 | 65.3 | 17 | 17.9 | 6 | 6.3 | 10 | 10.5 | |
| Only post treatment | 7 | 87.5 | 0 | 0.0 | 1 | 12.5 | 0 | 0.0 | |
| 2 | Profilactic treatment and protective equipment | 28 | 82.4 | 4 | 11.8 | 2 | 5.9 | 0 | 0.0 |
| Profilactic treatment and post treatment | 6 | 100 | 0 | 0.0 | 0 | 0 | 0 | 0.0 | |
| Protective equipment and post treatment | 13 | 81.3 | 0 | 0.0 | 2 | 12.5 | 1 | 6.3 | |
| 3 | Profilactic treatment and protective equipment and post treatment | 66 | 90.4 | 3 | 4.1 | 2 | 2.7 | 2 | 2.7 |
DISCUSSION
Main Findings
This was a retrospective survey among members of a Norwegian dental patient association with health complaints of which they attributed to former dental amalgam fillings. Most of the participants reported some degree of health improvement after amalgam removal, even though the mean degree of severity of symptoms was still high, with exhaustion and musculoskeletal complaints exhibiting the highest severity. This finding corresponds well with the fact that 37.6% of the participants reported poor to very poor current health. Improved health was most frequently reported among participants with the longest time interval since removal and with the highest number of precautions made in connection with amalgam removal.
Other Studies
The most commonly reported single symptoms in this study were tendency to rapid exhaustion followed by tiredness, concentration disturbance, and pain in joints and limps. This finding is in line with other Scandinavian studies in similar populations [12, 13, 24]. Lygre et al. [12] found that the most reported complaints were local symptoms around the mouth and general complaints such as pain from muscles and joints, fatigue and memory disturbance - a symptom pattern, which is confirmed in the present study. Moreover, half of the participants in our study reported pain in the face, a category, which included symptoms around the mouth as described in Lygre et al. [12].
Our finding of improved self-reported health in 74.4% of the participants after removal of amalgam, with 67.9% indicating major improvement or total recovery, is also in accordance with findings in other studies [8, 12-15]. Hanson reported better or much better health after removal of amalgam fillings in 73% of all participants across 25 studies (n=5821) [25]. A sum score of 35 on the GBB-24 complaint scale four to nine years after removal of amalgam, is somewhat higher than what was found in another Norwegian population 7 years after removal of amalgam, finding a sum score of 28.9 [13]. The higher mean complaint score in the present study might be related to the membership in a patient organization [26, 27].
Our finding of worsening of health in 8.4% (n=26) of the participants after removal of amalgam is in accordance with other studies. Long-term health deterioration following amalgam removal has been reported in 9.5% of the members in a Swedish patient organisation and in 13% of the patients examined at two different referral institutions [8, 28]. The differences in worsening of health across these studies may be related to differences in clinical settings. Similar deterioration rates were found in the present study of NDPA members (8.4%) and in the survey of members of the Swedish dental patient organisation (9.5%).
The reasons for worsening in self-reported health after amalgam removal are poorly understood. A study from a referral institution found that patients reporting health deteriorations had altered mercury concentrations in erythrocytes and plasma, compared to patients who reported improvement of health status after amalgam removal [29]. Sjursen et al. [30] concluded in a qualitative study that: “The dental amalgam was certainly important to get rid of, but it is uncertain how important the removal was for the experienced changes in health complaints”. Also Nerdrum et al. [13], who reported improvement of health after amalgam removal, state that the amalgam might not have been the main cause of the patient’s subjective health complaints. These statements together with the fact that the majority of the participants in this study still report complaints after removal of amalgam (and some even worsening of existing symptoms), suggest that a multifactorial explanation for the complex symptom pattern experienced by the patients cannot be ruled out. We did not collect information about, nor adjusted for, other chronic medical disorders in the studied participants.
The reason for the increased frequency of self-reported improvement of health over time is not obvious and is not in line with a study finding no difference in sum score on the GBB scale between 2 and 7 years after the removal [13]. As the main difference in the present study is found before and after one year since the removal of amalgam, one explanation may be that the body needs time to restore after the amalgam removal. Another explanation may be that the long recall time since removal in most of the groups could have led to inaccuracy in remembered health before removal.
The increased self-reported health associated with precautions taken during amalgam removal is interesting. This could be relevant for treatment procedures and for the recommendations from The National guidelines for assessment and treatment for suspected adverse effects from dental biomaterials [16] and the recommendations of NDPA [17]. It is, however not in line with a randomised controlled trial where no differences in health outcome were found between the groups where precautions (high doses of vitamins and trace elements, similar to our prophylactic treatment and post-treatment) were taken and the group where no precautions were taken [5]. This discrepancy can be related to different types and numbers of precautions, different settings and follow-up periods as well as differences in health status in the studied participants. Notably, in our study, health improvement increased with time since removal, suggesting that follow-up duration may be a relevant factor for assessed health change after amalgam removal.
Limitations
The main limitation of this study is the highly selected group of participants due to membership in a patient association and a rather low response rate. In order to identify patients with persistent health complaints attributed to former amalgam fillings (which was one aim of the survey commissioned by the Norwegian Directorate of Health), study participants were recruited from a specific patient association. The study population may therefore not be representative for the total patient group. Moreover, the only criterion for inclusion was that the patients had removed all their amalgam fillings. No information about possible clinical diagnoses was obtained. It is therefore not possible to distinguish study participants without a medical diagnosis from participants with a diagnosed medical condition.
The fact that no data were available on symptom load related to amalgam before removal of dental fillings, limits the results to symptoms remaining after amalgam removal. The majority of the participants had replaced their amalgam fillings more than nine years ago, so recall bias, meaning some inaccuracy reporting the experienced health changes cannot be excluded. Recall bias may therefore have influenced the reported differences in self-reported changes in health.
The low response rate (36.4%) may be a threat to the validity for the results of this study, because non-responders may differ significantly from those who responded. Our findings are, however in line with findings from other studies investigating symptoms and health changes in patients after removal of amalgam [25]. This might suggest that a potential non-response bias has not imposed a major threat to the validity of the results in the present study [31].
Clinical and Socio Economic Significance
Turner and Turk [32] suggest an improvement of 30% on a visual analogue scale as a clinically meaningful outcome. 74% of the participants in our study reported improvement of symptoms after amalgam removal on a 3 point categorical scale (improved-, unchanged-, or worsening of health), an outcome which is thus most likely clinically meaningful for the individual patients. The data show a linear connection between symptom load and perceived health status and are therefore in line with data from other patient groups with a similar symptom load. Since the absolute complaint load is a predictor of functional outcome [33, 34], these results are socioeconomically highly relevant [1, 2]. Even though patients in the present study still report a substantial symptom load after removal, the reported changes in experienced healthiness are of importance in the light of a health economic perspective.
Possible Interpretations
The experienced improvement of health was lowest within the first year after amalgam removal; it increased substantially after the first year, and was still continuously high several years later. It is not possible to conclude from a cross-sectional survey, which reflects just one point in time, the possible reasons for this. Some possible hypothesis may, however, be discussed.
The fact that the treatment is complicated and expensive increases the probability for an expectation dependent placebo effect, which likely plays a role in many medical interventions [35, 36]. The placebo effect is reportedly stronger for devices and invasive procedures [37, 38], which are similar procedures to the removal of dental amalgam. The fact that the experienced improvement of health is directly dependent on the number of precautions taken, could account for a strong expectation dependent placebo effect. Thus, it cannot be excluded that the placebo effect played a role in the evaluation of health status, the experienced improvement in health could likewise be related to possible biological effects of the precaution measures. It is impossible to draw conclusions on the issue of potential mediators of the effect from this survey. Only a prospective, controlled, interventional trial could elucidate the possible health related effects of amalgam removal. Nonetheless, more than 70% of participants reported improved health after amalgam removal at one to four years after removal, and the effect was still stable after more than ten years.
CONCLUSION
Most of the participants in this study reported a substantial improvement of health after amalgam removal. However, they still suffer a variety of complaints. Since absolute complaint load is a robust predictor for general outcome and socioeconomic burden for society, a possible intervention, which enables patients to further improve their health status, is desirable.
The findings in this survey are in line with a multifactorial origin of persistent health complaints attributed to former dental amalgam fillings in members of dental patient associations: The experienced improvement of health increased over time after removal and was linearly dependent on the number of precautions taken. The latter effect is compatible with potential placebo effects as well as biological effects.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank the leader and the administration of NDPA for posting the questionnaires to their members. Subsequently, we are grateful to the members of NDPA who filled in and returned the questionnaires. The study was funded through a grant from the Norwegian Directorate of Health. A special thanks to Liljan Smith Aandahl, retired Senior Advisor at the Norwegian Directorate of Health, who was instrumental in setting up the project for people with suspected adverse effects from dental amalgam, which this study is part of.


