All published articles of this journal are available on ScienceDirect.
Radicular Perforation Repair with Mineral Trioxide Aggregate: A Case Report with 10-Year Follow-up
Abstract
Background:
Iatrogenic complications such as accidental perforation of the root or the floor of the pulp chamber may occur.
Case Report:
Patient was referred for root canal retreatment of the mandibular left second molar with periapical lesion evidenced through radiographic examination. During post removal, iatrogenic perforation occurred at the mesial face of the distal root. After clinical localization of the perforation and bleeding control, MTA was applied. In a second appointment, the root canal filling was removed and the chemical-surgical retreatment of the canals was performed, followed by the obturation with gutta-percha and sealer. Patient returned after three days reporting no pain. After 6 months, 3, 7 and 10 years of follow-up.
Conclusion:
Absence of pain, normal periodontal probing and lack of radiolucent area at the region of perforation and the periapices were detected, which evidenced the successful repair of the tooth.
INTRODUCTION
Although endodontic treatment has a success rate of over 95%, iatrogenic complications such as accidental perforation of the root or the floor of the pulp chamber may occur, mainly in cases of root canal retreatment in which intraradicular posts need to be removed. If the iatrogeny is not properly treated, periodontal inflammation and ultimately the loss of the tooth may occur [1-3]. Caries evolution, resorption and the use of manual or rotary instruments may also cause root perforation, thus producing the communication between the tooth and the periodontal tissues [4]. The result is a chronic inflammatory reaction of the periodontium (characterized by the formation of granulation tissue) that can lead to irreversible loss of attachment or loss of the tooth [1].
The prognosis of perforations depends on the location, size and time of contamination of the lesion [1]. Such may have a favorable prognosis when correctly diagnosed and the treatment is performed with materials that present good sealing capacity and biocompatibility [5, 6]. The longevity of these restorations is a fundamental goal for the clinicians and also important for the patients [7, 8]. Moreover, the material should provide stimulus for the formation of hard tissue at the area of perforation, be radiopaque and non-resorbable [9]. After perforation the diagnosis and control of bleeding, a material must be inserted into the piercing region [1-3]. Mineral trioxide aggregate (MTA) was introduced in 1993 as a retrograde filling material with chemical, physical and biological properties superior to those found in other materials such as amalgam [9]. Besides the retrograde filling application, it has also been regarded as an ideal material for perforation repair, pulp capping, pulpotomy and apexification [10, 11]. It is available as a gray or white powder composed of mineral oxides, which are responsible for its chemical and physical properties [3,12]. The powder consists of fine hydrophilic particles whose main components are tricalcium silicate, tricalcium aluminate, tricalcium oxide and other mineral oxides. Because MTA has a pH of 12.5 after setting, constant calcium release and good antimicrobial activity have been reported [13].
In addition, MTA has an efficient marginal adaptation and sealing ability, avoiding bacterial penetration [2, 6, 13, 14]. According to Torabinejad et al. [12] (1995) the relatively low bacterial leakage observed when MTA was used as repair material was a result of its sealing ability rather than any antimicrobial properties of the material. These properties are essential in cases of teeth with resorption and furcal or radicular perforation [3, 15]. The repair of furcal perforation using MTA has been reported with both clinical and radiographic success [1, 14]. Through a long-term follow-up, the purpose of the present case is to present a successful treatment of an iatrogenic radicular perforation of a permanent mandibular second molar using MTA.
CASE REPORT
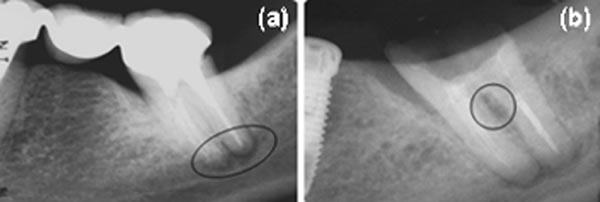
Forty eight-year old female patient was referred for root canal retreatment of the mandibular left second molar with periapical lesion. During anamnesis, patient complained of pain on mastication. The tooth was a pillar of a three-element bridge and did not respond to sensitivity tests. Periodontal probing was considered normal and radiographic examination revealed a small radiolucent area at the periapical region of the tooth (Fig. 1A). The treatment plan comprised of crown and metallic post removal and retreatment of the root canals of the second molar. During post removal, iatrogenic perforation of the mesial face of the distal root occurred (Fig. 1B).
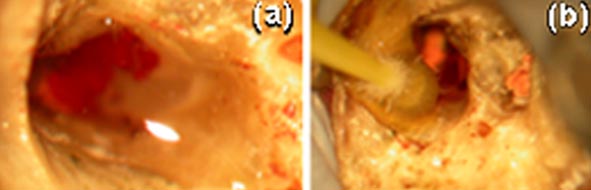
Rubber dam isolation of the tooth was performed and the root perforation was assessed (Fig. 2A) and treated under high magnification microscope (Carl Zeiss®, Oberkochen, Germany). Bleeding was controlled with copious irrigation with 1% sodium hypochlorite and application of hemostatic agent (ViscoStat®, Ultradent, Utah, USA) for 2 minutes (Fig. 2B).
The perforation was sealed with MTA-sterile saline paste (ProRoot MTA, Dental Tulsa; Dentsply®, DeTrey Konstanz, Germany) mixed in a 3:1 proportion. The paste was applied with a thin instrument (IPC-L, Cosmedent®, Chicago, USA) and adapted with a microbrush applicator moistened in distilled wa. The tooth was filled with a temporary restoration material (Cavit-G®, 3M ESPE, St. Paul, Minnesota, USA).
In a second appointment, after seven days, the root canal filling was removed with eucalyptol-based solvent, Gates-Glidden burs (Dentsply Maillefer®, Ballaigues, Switzerland) and K-files (Dentsply Maillefer®, Ballaigues, Switzerland). The working length was determined by using an apical locator (Root ZX, J. Morita®, Kyoto, Japan) and confirmed by periapical radiography root canal length measurements that also showed MTA in the drilling region (Fig. 3A).
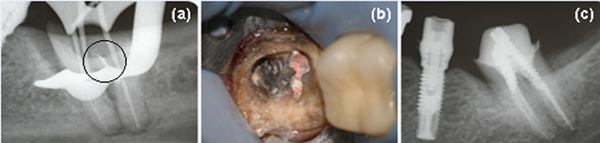
All canals were instrumented using crown-down technique with Gates-Glidden drills #2 and #3 in the preparation of coronal and medium third and #30 and #35 files for the final preparation of the mesial and distal canals, respectively. The procedure was performed with copious irrigation with 1% sodium hypochlorite and ethylene diamine tetra acetic acid (EDTA®, Formula e Ação, São Paulo, SP, Brazil). The canals were dried with sterile paper points and obturated with gutta-percha points and AH 26® (Dentsply, DeTrey Konstanz, Germany) sealer using the lateral condensation technique (Fig. 3B and C). Tooth was restored using an intracanal post and metal-ceramic crown. The patient returned after three days reporting no pain.
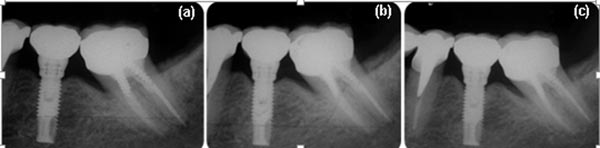
After 6 months, the tooth remained asymptomatic. Clinical examination showed absence of pain, no response to sensitivity tests and normal periodontal probing. After three, seven and ten year, the tooth remained asymptomatic and in function. Periapical radiographies revealed absence of radiolucent area at the region of perforation and the periapices during follow-up appointments (Fig. 4A, B and C). Through the examination of Cone Beam Computed Tomography (CBCT) scans, absence of radiolucency at the region of perforation and periapices was confirmed (Fig. 5A and B).

DISCUSSION
Radicular perforations, either iatrogenic or pathological, may make it impossible to keep the tooth in the oral cavity. Successful non-surgical endodontic procedures are related to the severity, location and size of the injury, the contamination of the site and the material employed [14]. Perforations affect the prognosis of endodontic treatments, and the immediate sealing of the perforation is a critical factor for the therapeutic success. Besides inadequate materials adversely contribute to the repair [1, 3, 14, 16, 17]. Therefore, the sealing of the perforation should be performed with biocompatible material, in order to provide a favorable environment for repair, and with characteristics similar to those of the dental hard tissue after setting [17-19]. In the present case, the immediate treatment with MTA of the perforation, a regenerative material, allowed a successful outcome, which could be clinically and radiographically confirmed over a ten-year follow-up period.
The main purpose of the therapeutic of perforations is to control and heal the inflammatory process [16]. Materials as amalgama, composite resin and glass ionomer cement were widely used in cases of perforations in the past; nowadays, MTA and BiodentineTM® have been used for this purpose [20, 21]. Studies have shown that MTA present better features, such as: alkaline pH, which inhibits bacterial activity; sealing ability, which avoid microbial infiltration; and low toxicity to the periodontal tissues [1, 22, 23]. Due to its hydrophilic feature, moist environment provides adequate condition to activate the chemical reaction of MTA, which is of great importance mainly for surgical procedures, since moisture is always present is such cases [24, 25]. Additionally, biocompatibility was tested in perforations of dog’s teeth, and the ability to induce the formation of hard tissue at the site of perforation was detected [26].
MTA is mostly composed of calcium and phosphate ions, which are also present in the tooth structure [13]. Due to its similarity of composition with dental hard tissues, it is believed that MTA is able to form hydroxyapatite when releasing calcium ions, thus allowing the sealing of perforated cavities. Besides, it has osteogenic and cementogenic potential, thus making it an excellent choice in cases of radicular perforation [27].
Most of the studies with MTA are based in animal or in vitro findings. Hence, long-term clinical investigations should be performed. Here, we presented a long-term follow-up of the healing of a radicular perforation, confirmed by the absence of periradicular radiolucent lesion, pain, and swelling along with functional tooth stability. In addition, technological advances such as the use of microscope, eletronic apex locator and regenerative materials allowed more controlled and predictive procedures.
CONCLUSION
The immediate treatment with MTA of an iatrogenic radicular perforation allowed the successful repair of the tooth, which remained asymptomatic, and with signs of normality over a ten-year period.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors do hereby thank FAPEMIG and UNIFAL-MG for the support regarding the publication of this case report.


