Comparing the Outcomes of Conventional Coronectomy and Graft Coronectomy: A Systematic Review
Abstract
Introduction:
Coronectomy is a widely accepted alternative surgical treatment modality in which only the crown of an impacted tooth is removed, leaving the roots and their associated nerve untouched. Uncertainty remains regarding whether intraoperative bone grafting of the coronectomy socket can reduce the incidence of typical postoperative procedure-related complications.
Objective:
The purpose of this literature review is to compare the outcomes of conventional coronectomy (CC) and grafted coronectomy (GC) in terms of whether adding a bone graft material after coronectomy of impacted mandibular third molars would decrease the incidence of typical complications.
Methods:
A total of 13 cases identified from electronic databases were included in this review based on their clinical relevance.
Results:
In general, there were no significant differences between conventional coronectomy and grafted coronectomy regarding the incidence of postoperative morbidities. However, grafted coronectomy with the placement of a bone graft material in the coronectomy socket could significantly decrease the incidence of root migration requiring re-operation of the exposed roots and reduce the preexisting pocket depth distal to the 2nd molar, especially in patients with mesioangular, impacted or horizontal wisdom teeth.
Conclusion:
According to the existing literature, grafted coronectomy might offer better clinical outcomes and can minimize the typical procedure-related drawbacks of conventional coronectomy while having similar surgical morbidities.
1. INTRODUCTION
Extraction of an entire wisdom tooth under certain circumstances is no longer recommended. An alternative should be performed to minimize the risk of temporary or permanent inferior alveolar nerve (IAN) neuropathy. The alternative procedure is coronectomy, which is a surgical procedure to remove the crown of the tooth while leaving the roots and their nerve untouched [1]. Coronectomy is considered when one or more specific radiographic signs show the proximity of the 3rd molar roots to the inferior alveolar nerve. These signs are darkening of the roots, narrowing of the root, interruption of the inferior alveolar canal, displacement of the canal, and narrowing of the canal. These signs are evaluated and confirmed by radiography, specifically cone-beam computed tomography (CBCT); this modality has better image quality, better measurement accuracy, and less distortion than other radiography techniques and, importantly, allows for visualization of the region of interest without overlap with other structures [2]. Although coronectomy is a treatment approach for reducing neurological impairment, it has two unfavorable complications. The first common complication is related to the position of the impacted teeth. A preexisting pocket distal to the 2nd molar can lead to bone resorption associated with a deep and abnormal tooth position, specifically in mesioangular and horizontal impaction patients. The second specific complication is root exposure as a result of root migration that requires a 2nd surgery to remove the remaining roots. Some studies have suggested filling the site with a bone graft to improve bone ossification and minimize the chance of developing complications. The purpose of this literature review is to compare the outcomes of conventional coronectomy (CC) and grafted coronectomy (GC) in terms of whether the addition of a bone graft material after coronectomy of impacted mandibular third molars would decrease the incidence of typical complications such as deep periodontal pockets distal to the second molars and migration of the remaining roots.
2. METHODS
This Systematic review is reported by the Preferred Reporting Items for Systematic review and Meta-analyses (PRISMA) guidelines [3]. The study protocol was not registered.
2.1. Search Strategy
Based on conventional coronectomy and grafted coronectomy as the key concepts and several alternative terms, the basic search strategy covered the following terms: coronectomy, partial odontectomy, intentional root retention with and without bone grafting, socket graft and PRF. The search was limited to in-human studies published in English. There were no restrictions regarding study design and date of publication in the electronic search. The following databases were searched to identify articles published during the indicated time period until 2022: PubMed, Cochrane library database and Elsevier-NYU library. The full search strategies for each database are shown in the Supplementary Material.
2.2. Inclusion Criteria
The following studies were included in this literature review: pilot randomized controlled trials (RCTs), preliminary reports of histological evaluations, retrospective studies, randomized controlled trials (RCT), case reports, and case series. Similarly, the inclusion criteria were patients requiring removal of at least one mandibular third molar tooth, comparison of conventional coronectomy with grafted coronectomy, complete tooth extraction, and use of a socket graft or platelet-rich fibrin (PRF). To be included, a study must have evaluated the risk of IAN damage, the periodontal pocket distal to the mandibular second molar, root migration, root exposure, and postoperative surgical morbidities.
2.3. Data Extraction
The following data were extracted from each of the included studies: patient characteristics; perioperative surgical management; study design; the number of patients and third molars in each treatment group; angle of the impacted third molar; type of graft material and membrane usage; timing and duration of follow-up; incidence of postoperative infection and pain; and need for reoperation.
2.4. Quality Assessment
According to the PRISMA statements, the evaluation of the methodological quality indicates the strength of evidence provided by the study because methodological flaws can result in biases. For randomized clinical trials, according to the Jadad scale [4], this procedure provides a total score ranging from 0 to 5, where 0 is a low-quality study and 5 is the highest possible quality. A trial is considered to have good quality when it gets a score of at least 3. According to the JBI's tool for assessing case series within the tool, some of the items relate to the risk of bi. In contrast, others relate to ensuring adequate reporting and statistical analysis. A response of “no” to any of the following questions negatively impacts the overall quality of a case series. For example, questions 1, 4, and 5 can be considered signaling questions for the domain “bias in the selection of participants into the study”; questions 2 and 3 for the domain “bias in the measurement of outcomes”; questions 6 and 7 for the domain “bias in the selection of the reported results”; and question 8 for the domain “bias due to missing data [5].
2.5. Risk of Bias in Individual Studies
Selection bias (retained allocation concealment), performance and detection bias (blinding of participants and operators), attrition bias (patient dropout, wash-out period of cross-over trials and missing values or participants and too short duration of follow-up) and reporting bias (selective reporting, unclear eliminations, and missing results) were recorded, evaluated and allocated according to Cochrane guidelines [6].
3. RESULTS
3.1. Study Selection
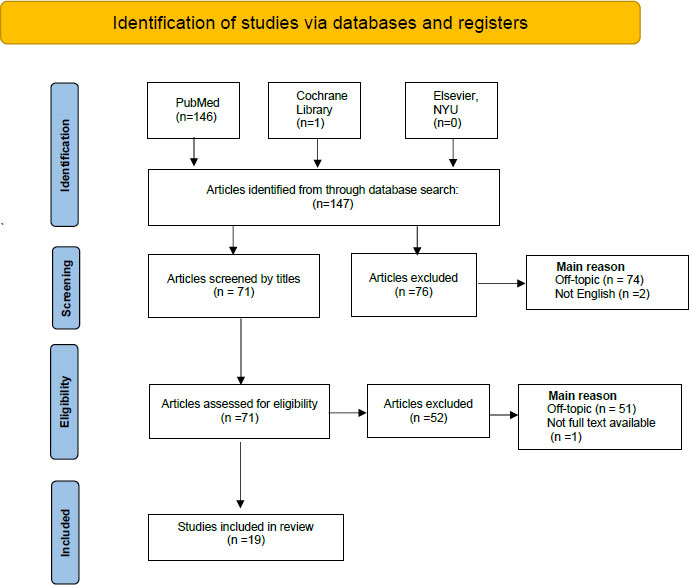
The following databases were searched to identify articles published during the indicated period until 2020: PubMed database n=146, Cochrane library database n=1, and Elsevier-NYU library n=0. A total of 147 articles were selected. These articles were split equally between two authors for evaluation purposes. First, the following articles were excluded after reading the titles: off-topic: n=74; and not in English: n=2. A total of 65 articles remained after reading all of the titles. Second, the following articles were excluded after reading the whole abstract: full text not available: n=1; and off-topic: n=51. A total of 19 articles remained after screening all abstracts (Fig. 1).
| Author, Year, Study Type |
No of Patients; No of Teeth | Type of Impaction; No | Type of Bone Graft w/ or w/o Membrane | Follow-up Time Weeks to Months |
Failure Rate | ||
|---|---|---|---|---|---|---|---|
| Root Migration | Changes in Pocket Depth Distal to MSM | Root Exposure | |||||
| I-Yiu Yan Leung, 2016. Pilot clinical trial with split-mouth randomization. |
n=6; 12 | Vertical=1 Horizontal= 4 Mesioangular=7 |
Bovine bone substitute 0.5-1 g w/ resorbable bilayer collagen membrane. | 2 W, 3 M, 6 M, and 12 M. | 1 mm | Statistically insignificant |
No |
|
SG n=6 |
|||||||
|
CG n=6 |
- | 3 mm | Statistically insignificant |
No | |||
| II-Yiu Yan Leung, 2018. Double-blind, parallel-group clinical trial with balanced randomization (1:1). |
n=48; 96 | Vertical n=2 Horizontal n=23 Mesial n=22 Distal n=1 |
0.5-1 g bovine bone substitute w/ resorbable bilayer collagen membrane. | 2 W, 3 M, 6 M, and 12 M, up to 2 years. |
1 mm | Statistically insignificant |
No |
|
SG n=48 |
|||||||
|
CG n=48 |
Vertical n=4 Horizontal n=18 Mesial n=24 Distal n=2 |
- | 3.5 mm | Statistically insignificant |
No | ||
| III-Michael Leizerovite, 2013. Case series. |
16; 20 | Class II=25 Class III=15 Class III=5 Class A=2 Class B=8 Class C=9 |
Resorbable hydroxyapatite, no membrane. |
Every 6 M, up to 2 years. | No | Improved | No |
| IV-Michael Leizerovite, 2013. Case report. |
1 | - | - | - | No | Improved | NA |
| V-Jeffrey A. Elo,2017. Retrospective study. 2006-2012 |
78; 92 | Mesioangular, horizontal, distoangular |
1.0 to 1.2 ml of mineralized corticocancellous allograft. | Yearly, up to 5-9 years | No | Improved | NA |
3.2. Study Characteristics
Different studies with varying designs and large sample sizes were conducted, and female and male patients were included. The pilot studies, clinical trials, and randomized split-mouth studies included bilateral 12 mandibular third molar teeth from a total of 6 patients; one side of the lower third molars was randomly selected to receive coronectomy with adjunctive guided bone regeneration (GBR) (study group) and the contralateral side (control group) received coronectomy only. The same authors performed the double-blind, parallel-group clinical trial with balanced randomization, and identical techniques were used. However, the sample size was increased to 48 patients and 96 teeth. Nonetheless, the results were almost the same. The grafting material used was 0.5-1 g bovine bone substitute with a resorbable bilayer collagen membrane. A case report and case series performed by the same author were also included; these studies involved 16 patients, 4 of whom had bilateral impacted mandibular third molars, and 12 had unilateral impaction, for a total of 20 teeth. All of the sockets were grafted with resorbable hydroxyapatite; no membranes were used. Additionally, a retrospective study included 78 patients, 14 of whom received bilateral grafted coronectomy while 64 received unilateral grafted coronectomy, for a total of 92 teeth. 1.0 to 1.2 ml of mineralized corticocancellous allografts were used for these patients. Furthermore, the existing clinical studies used various grafted materials, although the differences among grafted materials were not addressed. All of the studies included the following types of teeth impaction: mesioangular, horizontal, and distoangular (Table 1). Conversely, three RCTs were conducted for the same purpose with different surgical techniques. These studies investigated using xenografts to reduce osseous defects distal to the second molar after full extraction of impacted 3rd molars. Each study had a different sample size, ranging from 12 to 28 patients.
3.3. Preoperative/Postoperative Measures
Preoperative preparation was performed in each study group to facilitate reattachment and graft success, including scaling and debridement. Demineralization with tetracycline or 25% citric acid on the distal surface of the second molar was performed only in the case series and case report. In contrast, the RCT studies did not include preoperative preparation. However, the author did not mention the exact timing of when SRP should be performed. Furthermore, postoperative antibiotics were routinely prescribed and analgesics were used in all the included studies.
3.4. Quality Assessment
According to the Jadad scale for RCT (n = 2), the authors evaluated the quality of one clinical trial included in the qualitative synthesis based on five questions that analyze the randomization process, the experimental blinding, and the dropout rate, i.e., the patients lost to follow-up. In the evaluation of the quality of RCTs the total score of this study was 4, indicating a good quality study (Table 2). According to the JBI's tool for assessing case series studies (n = 1), the authors evaluated the qualities of one case series, based on ten questions. Questions 4, and 5 can be considered signaling questions for the domain “bias in the selection of participants into the study” the author only reports 20 patients who accept to be enrolled which impacts on the reliability of the study. The studies that indicate consecutive and complete inclusion are more reliable than those that do not. In addition, the author doesn't mention the statistical test used in the article (Table 3).
3.5. Study Outcomes
The existing clinical studies have been performed with different study designs, large sample sizes, a variety of grafting materials, and long follow-up periods. However, similar postoperative surgical morbidities have been observed between grafted coronectomy and conventional coronectomy. Grafted coronectomy can significantly decrease the incidence of root migration and minimize the preexisting pocket depth (Table 1). Patients with mesioangular full-bony impaction tended to have the deepest preexisting pockets. On the other hand, articles on surgical techniques for full mouth extraction have reported controversial results. Junior showed no significant difference between the study and control groups regarding pocket depth. In contrast, Hassan significantly reduced the probing pocket depth after placing a xenograft material. De Melo showed that using a xenograft did not improve the probing depth, although the radiography findings showed improvement in the periodontal defect.
| S.No. | Author | II-Yiu Yan Leung 2016 | II-Yiu Yan Leung 2018 |
| 1 | Is the study described as randomized? | 1 | 1 |
| 2 | Is the study described as double-blind? | 1 | 1 |
| 3 | Is there a description of withdrawals and dropouts? | 0 | 0 |
| 4 | The method of randomization is appropriate? | 1 | 1 |
| 5 | The method of blinding is appropriate? | 1 | 1 |
| 6 | Total score= 1 = Yes; 0 = No. | 4 | 4 |
| III-Michael Leizerovite, 2013. | YES | NO | Unclear | Not applicable |
|---|---|---|---|---|
| 1- Were there clear criteria for inclusion in the case series? | YES | - | - | - |
| 2- Was the condition measured in a standard, reliable way for all participants included in the case series? | YES | - | - | - |
| 3- Were valid methods used for the identification of the condition for all participants included in the case series? | YES | - | - | - |
| 4- Did the case series have consecutive inclusion of the participant? | - | NO | - | - |
| 5. Did the case series have complete inclusion of participants? | - | NO | - | - |
| 6. Was there clear reporting of the demographics of the participants in the study? | YES | - | - | - |
| 7- Was there clear reporting of clinical information of the participants? | YES | - | - | - |
| 8- Were the outcomes or follow-up results of cases clearly reported? | YES | - | - | - |
| 9-Was there clear reporting of the presenting sites'/clinics' demographic Information? |
- | - | - | Not applicable |
| 10. Was statistical analysis appropriate? | - | - | Unclear | - |
4. DISCUSSION
A common postoperative complication is related to the position of the impacted teeth and the preexisting pocket depth distal to the 2nd molar. This is because bone resorption is associated with a deep and abnormal tooth position, especially in mesioangular and horizontal impaction patients. This literature review investigated the effects of placing a graft after partial odontectomy and extraction of fully impacted 3rd molars.
4.1. Coronectomy
According to the existing literature, using grafted material with coronectomy is highly recommended for mesioangular and horizontally impacted teeth associated with preexisting pockets to decrease the pocket depth as well as reduce the chance for root migration to avoid the need for a 2nd procedure to remove the exposed roots. Generally, preparing the graft site by performing scaling and root planing (SRP) before placing grafting material is crucial to facilitating reattachment and ensuring graft success. Grafted coronectomy might offer better clinical outcomes and can minimize the typical procedure-related drawbacks of conventional coronectomy while having similar post-surgical morbidities. Nonetheless, the existing clinical studies did not address the differences between grafting materials and the indications for membrane usage.
4.2. Full 3rd Molar Extraction
Several studies were conducted to explore if the use of a bone graft reduces the preexisting pocket after full 3rd molar extraction. One study by Junior (2018) [7] established that there was no significant difference between the study and control groups regarding the distance from the crest of the alveolar bone to the cementoenamel junction after grafting the sockets with xenogeneic bone. Another study by De Melo in (2015) [8] did not recommend the use of inorganic bone grafts (xenogeneic bone), as this bone material did not improve the probing depth in their study even though the radiographic findings showed a decrease in the periodontal defect distal to the 2nd molar. A study by Hassan (2012) [9] observed contradictory results to the previous studies. It demonstrated a reduction in the probing pocket depth distal to the 2nd molar after grafting the osseous defects with a xenograft and a membrane. Moreover, whether grafting the socket after a tooth extraction is necessary for different osseous conditions has been investigated. However, most of the studies were conducted on animals. For this reason, more clinical studies on humans are recommended [10-22].
4.3. Limitations
The reason behind the choice of bone graft material and the indications for membrane usage are not addressed in each article, so the most effective material remains unknown, as each article used a different bone graft material with or without a membrane. On the other hand, the full 3rd molar extraction studies indicated that grafting does not improve the pocket depth distal to the 2nd molar but does lead to a significant increase in bone density. Because more studies are needed to investigate if other bone graft materials are more beneficial than xenografts, the current study used xenografts only. Unfortunately, due to a small number of clinical studies, currently, there is only limited evidence on which to provide definitive recommendations regarding whether grafting material should be placed after coronectomy or full extraction of the 3rd molars. Thus, further studies are needed to provide strong evidence regarding this topic.
CONCLUSION
We can deduce from this article that coronectomy represents reassuring technique allowing the respect of the underlying noble structures, in particular the mandibular canal, and intraoperative bone grafting of the coronectomy socket can reduce the incidence of typical postoperative procedure-related complications. However, Participant populations in the trials and other studies may not be representative of the general population or even the population undergoing third molar surgery. Many trials excluded individuals who were not in good health, and several excluded those with active infection. Consequently, we are unable to make firm recommendations to surgeons to inform their techniques for Graft Coronectomy. The evidence is uncertain, though we note that there is some limited evidence that placing grafted coronectomy in the socket could significantly decrease the incidence of root migration requiring re-operation of the exposed roots and reduce the preexisting pocket depth distal to the 2nd molar, especially in patients with mesioangular, impacted or horizontal wisdom. Furthermore, there were no significant differences between conventional coronectomy and grafted coronectomy regarding the incidence of postoperative morbidities. The evidence provided in this review may be used as a guide for surgeons when selecting and refining their surgical techniques. Ongoing studies may allow us to provide more definitive conclusions in the future.
LIST OF ABBREVIATIONS
| CC | = Conventional Coronectomy |
| GC | = Grafted Coronectomy |
| IAN | = Inferior Alveolar Nerve |
| CBCT | = Cone-beam Computer Tomography |
| PRF | = Platelet- Rich Fibrin |
| RCT | = Randomize Control Trials |
| GBR | = Guided Bone Regeneration |
| SRP | = Scaling and Root Planing |
| n | = Number |
| W | = Week |
| M | = Month |
| SG | = Study Group |
| CG | = Control Group |
CONSENT FOR PUBLICATION
Not applicable.
STANDARD OF REPORTING
PRISMA guidelines were followed.
AVAILABILITY FOR PUBLICATION
The authors confirm that the data supporting the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


