The Lower Lip Profile Change During Total Distalization of the Mandibular Dentition
Abstract
Objectives:
This study aimed to determine the factors influencing the lower lip profile during Class III lower total arch distalization camouflage treatment.
Methods:
The cohort included 45 patients diagnosed with skeletal class III malocclusion. These patients underwent camouflage orthodontic treatment with lower arch total distalization. Lateral cephalograms were taken at the pretreatment and posttreatment stages. Cephalometric measurements were analyzed to unravel the influencing factors of the lower lip profile. This study defined new variables, i.e., CK and CKA, for detailed soft tissue analysis.
Results:
Novel soft tissue measurements presented in this study showed statistically significant changes after treatment. The CK angle and L1 to A Pog, L1 to NB, and IMPA were statistically correlated. Simple regression analysis was performed between variables. The formula was ΔCKA = 0.79(Δ L1 to NB) -1.6, and multiple regression resulted in ΔCKA = 0.5(Δ L1 to NB) – 0.42 (‘LL to Eline’, before treatment).
Conclusion:
The present study provided evidence that the lower lip evaluations, including the novel CKA and CKHA, were significantly related to the mandibular incisor position during total distalization of the mandibular dentition. The results demonstrated that clinically significant lip retraction could be obtained. Therefore, non-extraction with distalization must be suggested as the first treatment option in mild skeletal class III malocclusion patients.
1. INTRODUCTION
The standard for orthodontic treatment is shifting from a hard tissue-based treatment to a soft tissue-based treatment paradigm [1]. To establish a standard for soft tissue-based orthodontic treatment, several researchers have proposed the ideal anterior and posterior positions of the soft tissue of the face [2, 3]. In addition, Holdaway defined the harmony line (H-line) and H-angle based on the position of the upper lip relative to the soft tissue Na-Pog line and set the standard for the upper aesthetic value. The norm was 7-8 degrees [4]. A class III malocclusion is a skeletal disharmony in which the growth of the mandible is relatively more dominant than that of the maxilla. In addition, the incidence of class III malocclusion is much higher in Asians than in Westerners [5]. Compensation treatment is known as one of the representative treatment methods, along with orthognathic surgery for patients with skeletal class III malocclusion [5]. It is known that a good soft tissue position can be obtained through compensation treatment in patients with skeletal Class III malocclusion [6]. However, unlike orthognathic surgery, compensation treatment may cause an excessive labial tilting of the maxillary incisors and lingual tilting of the mandibular incisors [7-9].
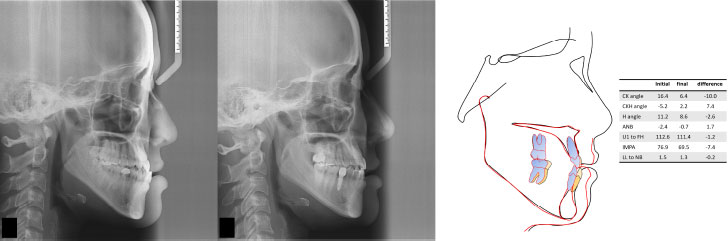
In many cases, mandibular extraction is necessary as part of the treatment plan to obtain an appropriate occlusion for a class III malocclusion. Recently, as an alternative to mandibular premolar extraction, class III malocclusion compensation treatment has been actively performed with total distalization of the mandibular arch using a TAD [10-13] (Fig. 1). Although such rearward movement of the mandibular arch has the advantage of being a possible treatment within the anatomical limitations, there has been no study that has determined whether the change in the anterior and posterior soft tissue position will be appropriately esthetic in the soft tissue-centered treatment planning paradigm described above. Excessive retraction of the lower lip also has the side effect of making the protrusion of the mandible more clearly visible. In evaluating class III malocclusions before and after treatment, the protrusion of the lower lip and the ratio of the upper lip should also be assessed.
The purpose of the present study was to evaluate the soft tissue index changes before and after treatment in patients who underwent class III malocclusion compensation treatment through total mandibular dentition posterior movement. Primarily, this study introduced new variables, CK angle (CKA) and CKH angle (CKHA), for detailed soft tissue analysis and aimed to analyze whether there is a correlation between the amount of lower incisor lingual movement and retraction of the lower lip employing known indicators and new CKA and CKHA. In addition, the usefulness of these two new variables for diagnosis and comparison before and after treatment was also estimated.
2. MATERIALS AND METHODS
2.1. Study Sample
Among the patients who visited the Department of Orthodontics, Institute of Oral Health Science, Ajou University School of Medicine, Suwon, South Korea, and received orthodontic treatment, 45 patients (average age, 26.8 years; 19-40 years old) who met the inclusion criteria of this study and did not meet the exclusion criteria were evaluated before treatment. Twenty-six females and nineteen males were selected.
Posterior lateral head radiographs were obtained.
The inclusion criteria were as follows:
1) Patients who were diagnosed with a skeletal class III malocclusion (ANB < 0˚),
2) Patients who had received class III malocclusion compensation treatment other than jaw surgery.
The exclusion criteria were as follows:
1) Patients with a history of orthodontic treatment,
2) Patients with impacted teeth,
3) Patients with a history of head and face trauma,
4) Patients with systemic disease that could affect tooth movements, such as clavicle dysplasia and cleft palate,
5) Patients with previous orthognathic surgery and anterior segmental osteotomy (ASO) surgery.
All patients were treated by the same orthodontist. The 0.022-slot MBT prescription bracket was used, mostly followed by a 0.016 nickel titanium, 0.018 ×0.025 Bioforce, and a 0.019 ×0.025 stainless steel wire sequentially. Temporary Anchorage Devices (TADs) were used in the posterior buccal shelf or retromolar area for posterior movement of the whole mandibular dentition. This study was conducted with permission and approval from the Institutional Review Board of Ajou University Hospital (IRB no.: AJIRB-MED-MDB-20-265).
2.2. Cephalometric Measurement
The obtained radiographs showed the patient in a natural head posture, and all radiographs were measured and analyzed by a researcher (BJ Kim) using V-ceph 8.3.0.3 (Osstem, Seoul, Korea) software. To verify the measurement error of the operator, all lateral radiographs were repeatedly measured at 4-week intervals, and the absence of errors was verified using Dahlberg’s formula [14].
Fourteen landmarks and seven reference lines were set for evaluation of the anterior-posterior position of the face before and after compensation treatment (Figs. 2 and 3). In this study, one line and two angles obtained were presented for the evaluation of the position of the lower lip at the initial visit and the position before and after treatment. The linear measurements are illustrated in Figs. (4 and 5) demonstrates the new lines and angles. In this study, the CK line was defined as a line connecting the soft tissue pogonion and the lower lip anterior (LLA) as a newly defined reference line. The angle between the CK line and the facial plane is defined as the CK angle (CKA) A, and the difference between the H-angle and the CK line is defined as the CKH angle (CKHA). A more protruded lower lip relative to the upper lip results in high negative values for the CKHA, which is similar to the ANB.




2.3. Sample Size Determination
Power analyses were performed using mean and standard deviation (SD) values of the angulation change of the lower incisor to the occlusal plane (mean, -2.8° and SD 3.6°) [15]. The R program (ver. 4.0.3, Vienna, Austria) suggested 16 as the minimum sample size with power = 0.9.
2.4. Statistical Analysis
The SPSS (IBM SPSS Statics Version 25) and R (4.0.3 version) programs were used for the statistical analysis of the measured values. The Shapiro–Wilk test was conducted and presented with the normality of data distribution of each variable. Paired t-tests with significance levels of 0.05 and 0.01 were performed to check whether the measured values changed before and after the compensation treatment.
Pearson’s correlation coefficients with significance levels of 0.05 and 0.01 were used to analyze the variables expected to be related to the change in measured values before and after compensation treatment. Afterward, simple regression and backward stepwise multiple regression analyses of the variables were also carried out.
3. RESULTS
SNA, SNB, and ANB were not significantly changed. Lower incisor retraction based on L1 to NB was -2.5±2.84 mm, and TVL with the lower lip retraction was -1.5 ±2.5 (Table 1). The hard-to-soft tissue response ratio was 1.7:1 (60%).
The results of paired t-tests (Table 1) showed statistically significant differences related to lower incisors before and after treatment for the values of ODI, APDI, and AB to the mandibular plane, Wits, IMPA, and L1 to A Pog, and L1 to NB. Among them, soft tissue factors related to changes in the lower lip, CKA, CKH, true vertical line (TVL), and TVL soft tissue B also showed statistically significant differences before and after treatment.
The results of a Pearson’s correlation analysis showed that before treatment, the lower lip to E line (“LL to E”) was also correlated with the retraction amount of CKA (P<0.01, r= −0.47). Initial lower lip protrusion quantity was associated with that of lower lip retraction.
Among the variables that exhibited treatment changes, the factors associated with CKA were investigated to evaluate which variables were correlated with lower lip profile. The results for the CKA showed a statistically significant correlation with L1 to A-Pog, L1 to NB, CKHA, Wits, IMPA, and APDI, and the CKH angle showed a statistically significant correlation with L1 to A Pog, L1 to NB, CKA, and IMPA (Table 2).
As a result of the regression analysis of “L1 to NB” and CKA, which can indicate the position of the mandibular incisors, the amount of change in CKA was positively correlated with the amount of change in L1 to NB [ΔCKA = 0.79(Δ L1 to N B) −1.6], R2 = 0.81, p<0.001.
In a multiple regression analysis, the relationship between the amount of change in CKA L1 to NB and “LL to E” (Initial value, Table 1) indicated that ΔCKA = 0.5(ΔL1 to N B) - 0.42(LLtoE) −1.48, R2 = 0.57, p<0.001.
| - | Initial Stage | Final Stage | - | ||
|---|---|---|---|---|---|
| Measurements | Mean | SD | Mean | SD | P value |
| ODI | 62.03 | 7.18 | 63.03 | 6.42 | 0.000** |
| APDI | 91.53 | 6.01 | 90.91 | 6.02 | 0.000** |
| AB to MPA | 62.22 | 6.51 | 64.03 | 6.42 | 0.000** |
| Wits | -7.32 | 4.47 | -5.61 | 3.33 | 0.000** |
| IMPA | 86.83 | 9.48 | 81.31 | 9.63 | 0.001** |
| L1 to Apog | 5.65 | 2.56 | 2.49 | 2.09 | 0.000** |
| L1 to NB | 5.56 | 2.95 | 3.18 | 2.42 | 0.000** |
| H angle | 11.70 | 5.24 | 11.19 | 4.47 | 0.192 |
| CK angle | 18.07 | 7.48 | 14.35 | 6.59 | 0.000** |
| CKH angle | −6.37 | 4.07 | −3.16 | 3.68 | 0.000** |
| TVL soft tissue A | −0.91 | 0.95 | −1.01 | 1.21 | 0.533 |
| TVL upper lip | 5.42 | 1.79 | 5.08 | 2.09 | 0.203 |
| TVL lower lip | 5.94 | 3.42 | 4.44 | 3.62 | 0.000** |
| TVL soft tissue B | 0.49 | 6.25 | 0.62 | 5.88 | 0.001** |
| TVL soft tissue pogonion | −0.88 | 4.85 | −2.03 | 4.69 | 0.688 |
| A’ to ULA | −6.34 | 1.80 | −6.09 | 1.85 | 0.242 |
| ULA to LLA | −1.95 | 1.86 | −1.84 | 1.33 | 0.639 |
| LLA to B’ | −6.83 | 2.77 | −6.47 | 2.10 | 0.182 |
| B’ to Pog’ | −2.13 | 1.80 | −2.74 | 2.00 | 0.001** |
| LLA to Pog’ | −5.85 | 3.71 | −4.36 | 2.59 | 0.000** |
| LL to E line | 1.03 | 2.88 | -0.57 | 2.36 | 0.000** |
| LL to NB | 5.38 | 2.90 | 2.88 | 2.42 | 0.000** |
| L1 to A Pog | L1 to NB | CK angle | CKH angle | Wits | IMPA | APDI | |
|---|---|---|---|---|---|---|---|
| L1 to A Pog | 1 | 0.868** (0.000) | 0.902** (0.000) | 0.319* (0.017) | −0.185 (0.177) | −0.937** (0.000) | 0.249 (0.067) |
| L1 to NB | 0.868** (0.000) | 1 | 0.927** (0.000) | 0.445** (0.000) | 0.001 (0.997) | −0.864** (0.000) | 0.007 (0.997) |
| CK angle | 0.902** (0.000) | 0.927** (0.000) | 1 | 0.449** (0.001) | −0.318* (0.018) | −0.907** (0.000) | 0.345** (0.010) |
| CKH angle | 0.319* (0.017) | 0.445** (0.000) | 0.449** (0.001) | 1 | −0.159 (0.249) | −0.332* (0.013) | 0.113 (0.409) |
Each value was obtained from the amount of change before and after the treatment.
4. DISCUSSION
Modern orthodontic treatment has been progressing as a paradigm of soft tissue-based treatment [1]. Holdaway published a baseline called the harmony line (H-line) and presented a standard for a harmonious appearance [4]. Subsequently, in a paper published in 1999, Arnett emphasized the importance of TVL based on a natural head position and announced the ideal soft tissue position using a method called soft tissue cephalometric diagnosis [2].
Camouflage treatment of skeletal class III malocclusion is the most suitable and realistic treatment method for patients who want nonsurgical treatment [16, 17]. The traditional method for class III malocclusion is to extract the mandibular premolars and then retract the mandibular incisors, which has a risk of root exposure or root resorption due to excessive retroclination [7-9]. A systematic study on soft tissue changes after extraction reported that lower lip retraction amounted to 2 mm to 4.5 mm based on “LL to Eline” in adult patients [17]. A class III research on increasing class III patients with lower second premolars extraction indicated that -2.8mm lower incisors retraction resulted in 0.9mm lower lip retraction [15]. After developing orthodontic TADs, posterior movement of the mandibular anterior teeth has been widely used as an alternative treatment to mandibular extraction for patients with class III malocclusion [10-13]. Obtaining an esthetic look with compensation treatment as good as expected with orthognathic surgery may be difficult, but patient satisfaction will be higher if soft tissue changes can be maximized [18]. However, it is difficult to predict the position before and after the treatment because the soft tissues of the face, including the lips, are viscoelastic [19].
This study aimed to determine the factors affecting the ratio of the lower labial protrusion to lower lip change with compensation treatment of class III malocclusions and quantify the expected retraction amount of the lower lip. The CKA, CKH angle, TVL, lower lip, TVL, soft tissue B, B’ to Pog’, and LLA to Pog’ showed statistically significant differences when the measured values before and after the treatment of patients who received the class III malocclusion compensation treatment were compared (Table 1). The rearward movement of the mandibular anterior incisor, which is currently mainly used for the compensation treatment of class III malocclusion, was strongly correlated with the amount of lower lip retraction, CKA (Table 2).
An additional regression analysis was performed on the CKA, which was found to be statistically correlated with L1 to NB, indicating the position of the mandibular incisors. An interpretation of the results suggested that the lower lip position, which changes according to the movement of the mandibular incisors, can be quantitatively predicted through the CKA. In other words, when the mandibular anterior teeth move 1 mm posteriorly, the lower lip can retrovert about 79% compared to the facial plane (N’-Pog’). This can be expected even with posterior movement of the mandibular incisors through non-extraction, suggesting that the mandibular full-arch distalization treatment will be highly effective in soft tissue changes.
In multiple regression analysis, ΔCKA = 0.5(ΔL1 to N B) − 0.42(LLtoE) −1.48. was formulated. The result explained that the protrusive lip retracted further, while the lower incisors moved backward, and the retraction ratio was 42%. When the initial lower lip protrusion became constant, a lower incisor, 1 mm retraction, resulted in 0.5° retraction of the lower lip (CKA). As the initial lower incisor position affected the initial lower lip position, the effect of lower incisor movement decreased when the lower lip became constant.
A limitation of this study is that it was conducted only on patients who had undergone treatment for posterior movement of the anterior teeth of the mandible, that is, non-extraction treatment. Although 3.7 mm retraction on average of the lower incisors presented significant lower lip retraction (2.1mm), which was comparable to the reported amount with extraction [ 15, 16], a comparison study with extraction or mandibular ASO will provide further insight into the differences and limitations between extraction and non-extraction treatments.
CONCLUSION
The results of this study showed ODI, APDI, and AB to be the mandibular plane. IMPA, L1 to A Pog, L1 to NB, and TVL, CKA, and CKHA were significantly correlated with lower incisor retraction in patients who underwent class III malocclusion compensation treatment. Among them, changes in the CK and CKH angles before and after treatment were correlated with L1 to A Pog, L1 to NB, CKA, and IMPA. The regression analysis results confirmed that the CKA could be predicted by the amount of mandibular anterior movement and initial lower lip position. Moreover, the amount of lower lip retraction was significantly correlated with that of lower incisor retraction during the treatment. The amount of the initial lower lip protrusion also influenced the lower lip profile change. Therefore, the CKA and CKHA newly presented in this study can be guidelines for soft tissue-centered diagnosis and treatment planning.
LIST OF ABBREVIATIONS
| LLA | = Lower Lip Anterior |
| SD | = Standard Deviation |
| TVL | = True Vertical Line |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the institutional review board (IRB) of the Ajou University Hospital (IRB No: AJIRB-MED-MDB-20-265).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were conducted following the ethical standards of the committee responsible for human experimentation (Institutional and National) and followed the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All the participants read and signed informed consent.
STANDARDS OF REPORTING
STROBE guidelines have been followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the https://github.com/pfChae/01042023.git, reference number 01042023.
FUNDING
None.
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.
REFERENCES
| [1] | Ackerman JL, Proffit WR, Sarver DM. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res 1999; 2(2): 49-52.[http://dx.doi.org/10.1111/ocr.1999.2.2.49] [PMID: 10534979] |
| [2] | Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthodon Dent Orthoped 1999; 116(3): 239-53. |
| [3] | Gianelly AA, Bednar JR. Bidimensional Technique: Theory and Practice. GAC International 2000. |
| [4] | Holdaway RA. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod 1983; 84(1): 1-28.[http://dx.doi.org/10.1016/0002-9416(83)90144-6] [PMID: 6575614] |
| [5] | Azamian Z, Shirban F. Treatment options for class III malocclusion in growing patients with emphasis on maxillary protraction. Scientifica 2016; 2016: 8150163.[http://dx.doi.org/10.1155/2016/8105163] |
| [6] | Burns NR, Musich DR, Martin C, Razmus T, Gunel E, Ngan P. Class III camouflage treatment: What are the limits? Am J Orthod Dentofacial Orthop 2010; 137(1): 1-9.[http://dx.doi.org/10.1016/j.ajodo.2009.05.017] |
| [7] | McFadden WM, Engstrom C, Engstrom H, Anholm JM. A study of the relationship between incisor intrusion and root shortening. Am J Orthod Dentofacial Orthop 1989; 96(5): 390-6.[http://dx.doi.org/10.1016/0889-5406(89)90323-5] [PMID: 2683733] |
| [8] | Kaley J, Phillips C. Factors related to root resorption in edgewise practice. Angle Orthod 1991; 61(2): 125-32.[PMID: 2064070] |
| [9] | Wishney M. Potential risks of orthodontic therapy: A critical review and conceptual framework. Aust Dent J 2017; 62: 86-96.[http://dx.doi.org/10.1111/adj.12486] [PMID: 27868202] |
| [10] | Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop 2015; 148(1): 22-36.[http://dx.doi.org/10.1016/j.ajodo.2015.04.012] [PMID: 26124025] |
| [11] | Jing Y, Han X, Guo Y, Li J, Bai D. Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am J Orthod Dentofacial Orthop 2013; 143(6): 877-87.[http://dx.doi.org/10.1016/j.ajodo.2012.05.021] [PMID: 23726338] |
| [12] | Yanagita T, Kuroda S, Takano-Yamamoto T, Yamashiro T. Class III malocclusion with complex problems of lateral open bite and severe crowding successfully treated with miniscrew anchorage and lingual orthodontic brackets. Am J Orthod Dentofacial Orthop 2011; 139(5): 679-89.[http://dx.doi.org/10.1016/j.ajodo.2009.07.023] [PMID: 21536212] |
| [13] | Chen K, Cao Y. Class III malocclusion treated with distalization of the mandibular dentition with miniscrew anchorage: A 2-year follow-up. Am J Orthod Dentofacial Orthop 2015; 148(6): 1043-53.[http://dx.doi.org/10.1016/j.ajodo.2015.03.034] [PMID: 26672711] |
| [14] | Houston WJB. The analysis of errors in orthodontic measurements. Am J Orthod 1983; 83(5): 382-90.[http://dx.doi.org/10.1016/0002-9416(83)90322-6] [PMID: 6573846] |
| [15] | Proffit WR, Fields HW Jr, Sarver DM. Contemporary Orthodontics. 5th. 5th.Elsevier 2012. |
| [16] | Leonardi R, Annunziata A, Licciardello V, Barbato E. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod 2010; 80(1): 211-6.[http://dx.doi.org/10.2319/010709-16.1] [PMID: 19852663] |
| [17] | Lin J, Gu Y. Lower second molar extraction in correction of severe skeletal class III malocclusion. Angle Orthod 2006; 76(2): 217-25.[PMID: 16539545] |
| [18] | Bailey LJ, Haltiwanger LH, Blakey GH, Proffit WR. Who seeks surgical-orthodontic treatment: A current review. Int J Adult Orthodon Orthognath Surg 2001; 16(4): 280-92.[PMID: 12390006] |
| [19] | Hodgkinson D, Firth FA, Farella M. Effect of incisor retraction on facial aesthetics. J Orthod 2019; 46(1_suppl): 49-53.[http://dx.doi.org/10.1177/1465312519840031] [PMID: 31056032] |


