All published articles of this journal are available on ScienceDirect.
Effect of the Diameter and Preparation Method of the Occlusal Screw Access Channel on Fracture Resistance of Cement-retained Implant-supported Posterior Monolithic Zirconia Crowns
Abstract
Background:
The favorable fracture resistance of implant-supported crowns is important. Zirconia crowns can be an acceptable treatment in relation to metal‒ceramic crowns for achieving the best clinical success.
Objective:
The present study evaluated the effect of the diameter and preparation method of the occlusal screw access channel on the fracture resistance of cement-retained implant-supported posterior monolithic zirconia crowns for their retrievability.
Methods:
Fifty-six implant-supported posterior multi-layer monolithic zirconia crowns were designed. Twenty pieces with an initial occlusal channel were designed with 2.3 and 3.5 mm diameters (n =10 each). In addition, 30 pieces with an intact occlusal surface as the control group or the crowns in which the occlusal channel was prepared with a bur were designed in 10 and 20 samples, respectively. Six additional crowns were also designed for SEM evaluations after their preparation with a bur.
Results:
The maximum fracture resistance value was recorded in the control group, followed by the initial access channel group with a 2.3 mm diameter. The minimum fracture resistance value was recorded in crowns with a 3.5-mm diameter hole prepared with a bur. The mean fracture strength in the groups with a 2.3 mm diameter was higher than in groups with a 3.5 mm diameter (P<0.05). Cracks in samples prepared with a bur were seen under SEM.
Conclusion:
This study showed that using an initial access hole with a diameter of 2.3 mm is the best choice in hybrid implant-supported crowns. However, when it is necessary to prepare an access hole with a bur, it should be done with the smallest possible diameter.
1. INTRODUCTION
Implant-supported zirconia crowns are an acceptable treatment choice in the anterior and posterior regions [1]. A suitable combination of strength, precision, color, and excellent biocompatibility allows using zirconia restorations in various clinical situations [1]. In addition, regardless of the type of design, zirconia crowns have a lower fracture rate than metal‒ceramic crowns [1]. Implant-supported prostheses are screw-retained or cement-retained, each having advantages and disadvantages [1-7]. In screw-retained crowns, due to the occlusal screw access channel, occlusal morphology, occlusion, aesthetics, and fracture resistance are adversely affected, and there are disadvantages such as screw-loosening or fracture, difficulty, high cost of the manufacturing process, and poor passivity [1-7]. On the other hand, among the advantages of screw-retained crowns, their retrievability and easy repositioning can be mentioned as their most important advantage [1-5]. The advantages of cement-retained crowns are ease and lower cost in manufacturing, better aesthetics, ideal occlusion, and passive adaption [1-5]. However, cement-retained crowns have some problems, such as difficult retrievability and the possibility of excess cement remaining [1-5]. Cement-retained crowns are the first choice, especially in aesthetic areas, although there are concerns due to their difficult retrievability [3]. Many studies have reported that preparation of the occlusal access channel with a bur in cement-retained crowns for their retrievability reduces their strength [1-5]. Since few studies are available on the effect of occlusal channel diameter on the fracture resistance of these restorations and currently, there are no accepted guidelines for determining the appropriate diameter of the occlusal channel [4], the present research evaluated the effect of diameter and preparation method of occlusal screw access channel on the fracture resistance of cement-retained implant-supported posterior monolithic zirconia crowns in terms of their retrievability.
2. MATERIALS AND METHODS
2.2. Determining the Sample Size
The results of Sabourie’s study [ 1 ] were used to determine the sample size. Considering 5% for type I error and 80% for the test power, the sample size in each group was estimated at n=5. The sample size was doubled, and finally, 10 samples were included in each group to increase the study’s validity; together with 6 crowns used for SEM analyses, a total of 56 samples were included.
2.3. Procedural Steps
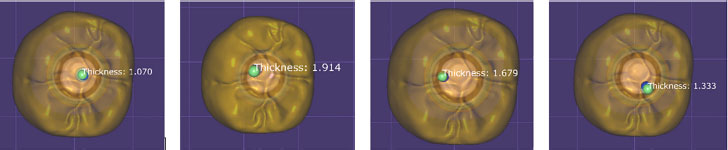
Fifty-six titanium cylindrical fixtures measuring 4.5 mm in diameter and 10 mm in length (Osstem, Seoul, South Korea) were mounted in auto-polymerized acrylic blocks (Vertex dental B.V., Soesterberg, Netherlands) using a dental surveyor (Marathon 103, Glendale, USA Meta Dental). The implant platform was placed 1 mm coronal to the resin. Fifty-six straight titanium abutments with a diameter of 4.5 mm and two cuffs (Osstem, Seoul, South Korea) were used. Abutments were scanned by an extraoral scanning device (Medit t300, Seoul, South Korea) to create a CAD model for the right mandibular first molar. Samples were designed with and without an occlusal access channel in full contour form with buccolingual and mesiodistal dimensions of 10 and 10.5 mm, respectively, and an occlusal surface thickness of 1-2 mm at the same height of the cusps (except the distal cusp which had a lower height than other cusps) by Exocad software (Gmbh, Darmstadt, Germany) (Fig. 1). In crowns with an initial occlusal channel, a computer model was designed with a hole at the center of the occlusal surface with 2.3 mm and 3.5 mm diameters, 10 pieces each (20 pieces in total). However, the computer model for the crowns without an access channel as the control group or the crowns in which the occlusal channel was prepared with a bur was designed as an intact occlusal surface with 10 and 20 samples, respectively (30 in total). In addition, six crowns with intact occlusal anatomy were designed to perform SEM analyses (MIRA3 FEG-SEM, Brno-Kohoutovice, Czech Republic) and evaluate surface defects caused by preparation with 2.3 mm and 3.5 mm diameter burs (Dia Tessin SG801, Losone, Switzerland). The diameters of 2.3 mm and 3.5 mm of the occlusal channel were chosen according to the diameter of the shank of the implant screwdriver (Osstem, Seoul, South Korea), which is about 1.8 mm, respectively, in a condition where the exact location of the abutment screw is known (diameter: 2.3 mm, 0.5 mm is larger than the diameter of the shank of the screwdriver to ensure freedom of movement of the screwdriver and not to become stuck to the walls of the access hole) and in a condition where the position of the screw abutment is not known. As a result, further extension of the access hole becomes necessary (diameter: 3.5 mm).
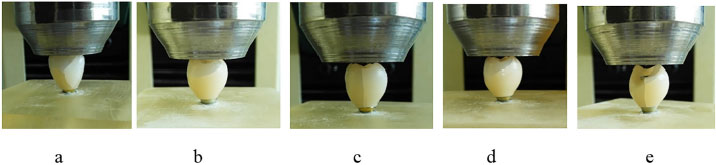
The crowns were milled from multi-layer zirconia blanks A2/A3 (Ceramill Zolid Fx Multilayer, Koblach, Austria Amann Girrbach AG) using a milling machine (Rainbow™ Mill-Zr, Seoul, South Korea Dentium). After sintering (Ceramill Therm 3 High-Temperature Furnance, Koblach, Austria Amann Girrbach AG) and glazing (Schaan, Liechtenstein Glaze Powder & Glaze Liquid, Ivoclar Viva Dent Inc.) according to the manufacturer’s recommendation (Fig. 2). The seating of the crowns and their marginal fitting on the corresponding abutment were controlled. The Pre-Op Model technique was used to achieve the same anatomy between crowns without occlusal holes and crowns with initial occlusal holes. First, a sample without an occlusal hole was designed, milled, and sintered; it was then placed on the corresponding abutment and scanned so that the crowns with the initial occlusal hole were designed according to it. After
sintering and before cementing, the crowns were cleaned in an ultrasonic device (Berlin, Germany, Bandelin Sonorex Super rk102 Plus) for ten minutes. According to the manufacturer’s instructions, the abutments were torqued on the fixtures with a force of 30 Ncm and sealed with gutta-percha (Meta Biomed, Chungcheongbuk-Do, Korea). Each crown was then cemented to the corresponding abutment so that in a group with an initial access channel (hybrid technique), before cementing, the hole was sealed by wax (Renfert GmbH, Hilzingen, Germany) [5]. According to the manufacturer’s recommendations, each crown was cemented to the corresponding abutment with zinc phosphate (Hoffmann’s Dental Manufaktur GmbH, Berlin, Germany). Excess cement was removed with a sickle scaler (Hu-Friedy Mfg Co, LLC, Chicago, USA). In all the samples, the cement was set while the crown was subjected, in its longitudinal axis, to a static force of 50 N (5 kg) for 10 minutes in a universal testing machine (Hounsfield UTM H5K-S, England).
After setting the cement and removing the excess cement, the occlusal holes were prepared with a bur in 20 pieces with an intact occlusal surface. All these channels were prepared by a new coarse-grit round diamond bur (Dia Tessin SG801, Losone, Switzerland) in a high-speed handpiece (Duisburg, Germany NSK Pana Air FX PAF SU B2 Air Turbine) at 200,000 rpm under air and water spray on the surveyor machine (Mariotti & C F18 Laboratory Milling Machine, Milan, Italy). To ensure that the diameter and position of the access channels prepared by the bur were similar to the initial access channels, first, two crowns with about a 2-mm extension of the initial access hole to the occlusal surface were designed and made, one with a diameter of 2.3 mm and another with a diameter of 3.5 mm (Fig. 3). Then, a guide pattern was made on them with a condensation silicone material with putty consistency (Coltene, Altstätten, Switzerland) (Fig. 4). In crowns with an initial access channel (hybrid technique), the wax plug (Renfert GmbH, Hilzingen, Germany) was removed from the hole. Then, the crown‒abutment complex in crowns with initial holes and with bur-prepared holes were examined under a stereomicroscopic (Nikon Digital Sight Ds-Fi1, Tokyo, Japan) at ×10 magnification to remove excess cement with a sickle scaler (Hu-Friedy Mfg Co, LLC, Chicago, USA) and cleaned with an ultrasonic device (Berlin, Germany, Bandelin Sonorex Super rk102 Plus) and water vapor pressure (Zhermack VAP 6, South Tyrol, Italy) to achieve a clean and non-contaminated surface and seal the occlusal channel with the composite.



The initial and bur-prepared occlusal holes were sealed with composite resin (3M, ESPE, Minneapolis, USA) according to the protocol recommended by the manufacturer. Conditioning the zirconia surface to seal the occlusal channel with the composite resin was carried out by sandblasting with 50-µm aluminum oxide particles under a pressure of 0.1 MPa from a distance of 10 mm at an angle of 90º, followed by applying a ceramic primer containing MDP and silane (Monobond Plus, Schaan, Liechtenstein Ivoclar Vivadent AG). Finally, an adhesive layer (Adhese Universal, Schaan, Liechtenstein Ivoclar Vivadent AG) was applied and cured for 10 seconds at a light intensity of 1200 mV/cm2 (Woodpecker, Guangxi, China).
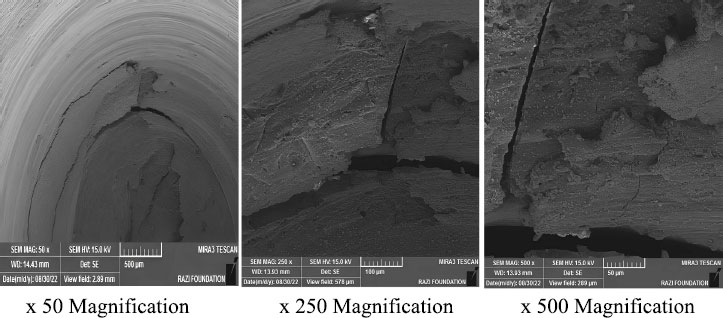
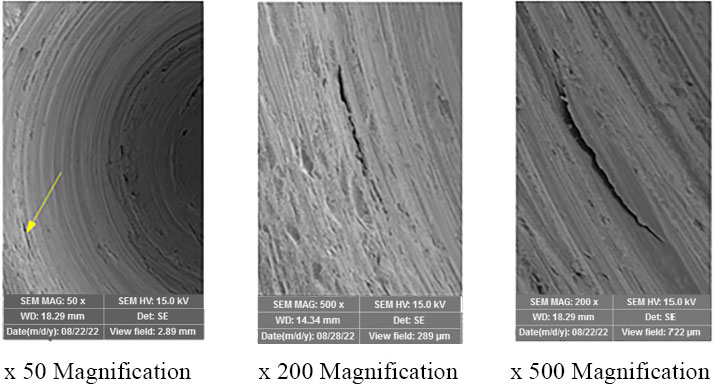
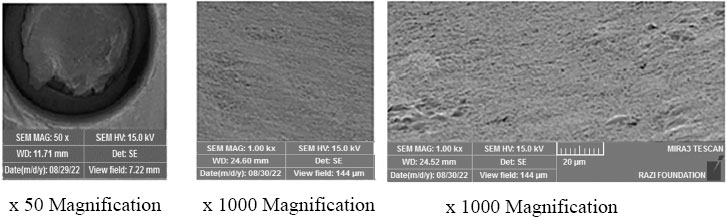
All the samples were kept in distilled water at room temperature for one week. Thermal cycling was applied using 1000 cycles at 5/55°C with a time interval of 30 seconds on all the samples (Nemo Mechatronica, Mashhad, Iran). The samples were loaded with static compressive force using a 20 mm diameter flat metal surface connected to the upper and movable head of the universal testing machine (Hounsfield UTM H5K-S, England) to perform the static compressive fracture resistance test. The force was applied along the longitudinal axis of the crown at a speed of 0.2 mm/min simultaneously to the tips of all four crown cusps (two buccal cusps and two lingual cusps with the same height, except the distal cusp, which had lower height than other cusps) until fracture occurred [3, 8]. Observation of cracks during compressive loading was considered a restoration fracture (Fig. 5). The force during restoration fracture was recorded in Newton (N) [1-3, 5-7]. The ISO reference was not used for the mechanical tests; these tests were outside the standard. Procedures and methods were based on previous studies that have been referenced. Six additional samples were prepared with 2.3 mm and 3.5 mm diameter burs (Dia Tessin SG801, Losone, Switzerland) with the same methods but were not loaded and were gold-sputtered using a sputtering machine (Emitech K 550, Emitech Ltd Ashford, Kent, UK) and then examined under SEM (MIRA3 FEG-SEM, Brno-Kohoutovice, Czech Republic) to investigate the surface damage caused by the bur in comparison to the initial ones [8].
2.4. Inclusion Criteria
1. Monolithic zirconia crowns without any cracks or structural problems.
2. The diameter of the access channel exactly matches the mentioned values (2.3 or 3.5 mm).
2.5. Exclusion Criteria
1. The presence of structural problems or cracks in the samples before testing.
2. Incompatibility of the channel’s diameter with the dimensions mentioned in the study (diameters other than 2.3 or 3.5 mm).
| The Study Groups | No. | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| A1 | 10 | 3260.93 | 720.17 | 2322.70 | 4488.00 |
| A2 | 10 | 2729.09 | 406.77 | 2128.00 | 3354.50 |
| B1 | 10 | 2245.62 | 688.20 | 1613.80 | 3298.30 |
| B2 | 10 | 1936.43 | 497.62 | 1333.20 | 2883.20 |
| C | 10 | 3436.74 | 900.22 | 2013.00 | 4520.30 |
| Total | 50 | 2721.76 | 861.84 | 1333.20 | 4520.30 |
Group A2 : An initial occlusal screw access channel with a diameter of 3.5 mm;
Group B1 : An occlusal screw access channel with a diameter of 2.3 mm, prepared with a bur;
Group B2 : An occlusal screw access channel with a diameter of 3.5 mm, prepared with a bur;
Group C : Control group (no occlusal screw access channel).
2.6. Data Analysis
The data were collected and analyzed using SPSS 17 with Tow-Way ANOVA, Independent T-Test, and One-Way ANOVA, followed by the Games-Howell post hoc tests.
To evaluate the groups more efficiently, they were coded as follows:
1) Group A1: An initial occlusal screw access channel with a diameter of 2.3 mm
2) Group A2: An initial occlusal screw access channel with a diameter of 3.5 mm
3) Group B1: An occlusal screw access channel with a diameter of 2.3 mm, prepared with a bur
4) Group B2: An occlusal screw access channel with a diameter of 3.5 mm, prepared with a bur
5) Group C: Control group (no occlusal screw access channel)
3. RESULTS
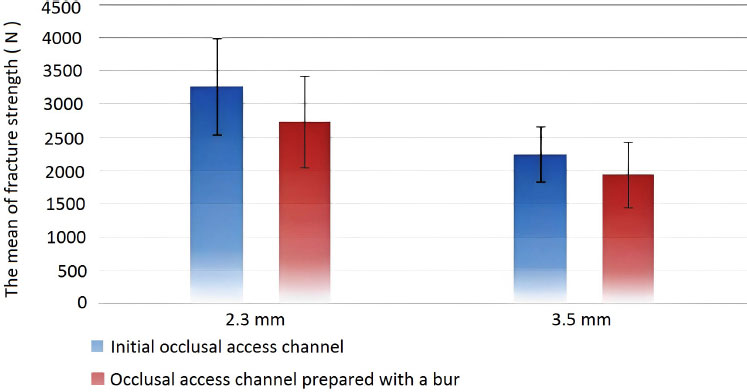
Table 1 presents the means and standard deviations of the fracture strength values in the two initial and access channels prepared by a bur with diameters of 2.3 mm and 3.5 mm.
Statistical analyses showed significant differences in the means of the fracture strength variable between the two access channel preparation methods, with higher mean fracture strength in the initial access channel than in bur-prepared access channels (P<0.001). Also, there was a significant difference in the mean fracture strength variable between the two diameters of 2.3 mm and 3.5 mm, with higher mean fracture strength in the 2.3-mm diameter (P<0.05). There was no synergistic effect between the access channel preparation method and the diameter; in other words, the effect of the access channel preparation method on the mean of fracture strength variable was the same in both diameters (P>0.05). However, in the same diameters, there was a significant difference in the mean fracture strength variable between the two access channel preparation methods, with higher mean fracture strength in the initial access channels than in the bur-prepared access channels (P<0.05) (Table 2 and Fig. 6). Examining the samples under the SEM confirmed the presence of significant cracks in the samples with bur-prepared access channels with diameters of 3.5 mm (Fig. 7) and 2.3 mm (Fig. 8) compared to those with initial access channels (Fig. 9).
| Diameter | Occlusal Access Channel | No. | Mean | Standard Deviation | P-value | |
|---|---|---|---|---|---|---|
| 2.3 mm | Initial | 10 | 3260.93 | 720.16 | .005* | .031** |
| Prepared with a bur | 10 | 2245.62 | 688.20 | |||
| Total | 20 | 2753.28 | 860.98 | - | ||
| 3.5 mm | Initial | 10 | 2729.09 | 406.77 | .001* | |
| Prepared with a bur | 10 | 1936.43 | 497.62 | |||
| Total | 20 | 2332.76 | 600.85 | - | ||
| Total | Initial | 20 | 2995.01 | 631.25 | <.001** | - |
| Prepared with a bur | 20 | 2091.03 | 605.64 | |||
| Total | 40 | 2543.02 | 763.13 | - | - | |
4. DISCUSSION
Comparing the advantages and disadvantages of cement-retained and screw-retained implant-supported crowns has been controversial for a long time [9]. Screw-retained crowns’ problems have decreased their use, including ceramic chipping, undesirable aesthetics, and failure to achieve ideal occlusion due to the presence of the occlusal channel. Furthermore, the most common problem of these prostheses is screw loosening [10]. On the other hand, retrievability is the most important advantage of these prostheses. Cement-retained crowns have become popular due to their advantages, including ease of fabrication, acceptable esthetics, passiveness, lower cost, easier access in the posterior regions, and biologically and functionally long-term clinical success [10]. However, cement-retained crowns have some problems, such as difficult retrievability and the possibility of excess cement remaining. Furthermore, failure to achieve success in the retrievability of cement-retained implant-supported crowns can force the clinician to cut the crown, which can damage the abutment, necessitating crown reconstruction [10]. Therefore, the present research evaluated the effect of the diameter and preparation method of the occlusal screw access channel on the fracture resistance of cement-retained implant-supported posterior monolithic zirconia crowns concerning their retrievability.
In the present study, the maximum fracture strength value was related to the C group, with a mean of 3436.74 N, followed by the A1 group, with a mean of 3260.93 N. The minimum fracture strength value was recorded in the B2 group with a mean of 1936.43 N. This study showed significant differences in the means of fracture strength values between the groups (P<0.01). The highest mean difference in samples with an occlusal channel was between A1 and B2 groups. Also, this study showed that the mean fracture strength of the groups with a 2.3 mm diameter was higher than in groups with a 3.5 mm diameter (P<0.05). However, from the fracture strength point of view, the preparation method of the access channel and its diameter had no synergistic effect on each other; in other words, the effect of the hole preparation method on the mean of fracture strength variable was the same in both diameters (P>0.05). In the same diameters, there was a significant difference in the mean fracture strength variable between the two access channel preparation methods, with higher mean fracture strength in the initial holes than in the bur-prepared holes (P<0.05). SEM observations confirmed the presence of cracks in bur-prepared access channel groups compared to the initial ones, confirming the statistical results of the present study. According to various studies, since the maximum bite force in the molar areas is 807 N in men and 650 N in women, all the groups in the present study were clinically applicable [11]. However, it should be kept in mind that the forces in the molar areas are not just a single vertical force, and other factors, such as oblique forces, aging, and fatigue fracture, should also be considered as variables that can be the subject of further studies in the future. Among other variables that can affect the study results are the type and the rate of the thermocycling process. The results of the present study are comparable with those of previous studies and are as follows.
Hussein et al. (2016) studied the effect of the occlusal access channel on the fracture strength of three types of implant-supported crowns. According to the results, monolithic zirconia crowns (Weiland Zenostar coping; Weiland dental+Technik GmbH & CO KG) had the highest fracture strength with a significant difference from lithium disilicate crowns (IPS e.max CAD; Ivoclar Vivadent AG) and veneered zirconia by IPS e.max Ceram. Also, although the preparation of the access hole decreased the fracture strength among the groups, its effect was not statistically significant (P>0.05) [5]. The study by Hussein et al. (2016) considered using monolithic zirconia as a desirable choice to achieve maximum fracture strength. Since preparing the access hole reduced the average fracture strength in the samples, it is consistent with the present study. However, considering the non-significance of the effect of preparing the access channel on the fracture strength, it is different from the present study. One of the reasons for this is the use of different materials, the different thicknesses of the crowns, and the difference in the access channel diameter.
Carrillo et al. (2020) studied the fracture strength of cement-retained, screw-retained, and hybrid implant-supported metal‒ceramic crowns in molar teeth. Thirty crowns were divided into three groups: cement-retained, screw-retained, and hybrid. The results showed that screw-retained crowns had minimum fracture strength, which was significantly lower than cement-retained and hybrid groups. There was no significant difference between cement-retained and hybrid groups in terms of fracture strength. The initial access hole did not significantly affect the fracture strength of the samples [ 12 ]. The results of this study are consistent with the present study concerning the reduced fracture strength following the creation of an initial occlusal access channel, with no significant difference between the group without the occlusal access channel and with the initial occlusal access channel in terms of fracture strength.
In another study by Derafshi et al. (2015) on the effect of the type of occlusal screw access channel design in cement-retained implant-supported metal-ceramic crowns, 36 implant-supported crowns were fabricated and divided into three groups of 12. The crowns of the first group were selected as the control group, and no access holes were made to them. In the second group, the occlusal access channel was prepared by a bur, and in the third group, an initial occlusal screw access channel was designed and created. After thermocycling, the samples were loaded in a universal testing machine at a speed of 2 mm/min, and their fracture resistance was evaluated. The results showed no significant differences between the groups (P>0.05) [ 3 ]. The results of this study differed from the results of the present study. The reason for the discrepancy can be the high speed of applying force (2 mm/min) on the samples. Also, the sample materials in the studies were different, which could be one of the other reasons for the inconsistent results.
Mokhtarpour et al. (2016) studied the effect of the occlusal hole preparation method on the fracture strength of implant-supported maxillary central monolithic zirconia crowns (White-peaks, Copran Zr-i, Wesel, Germany). Samples were evaluated in three groups. In the first group, the access hole was not prepared. In the second group, the initial hole was designed with CAD. In the third group, the access hole was prepared with a bur after zirconia sintering. The diameter of the hole was the same in the second and third groups. The results showed that the fracture strength of the first group was significantly higher than other groups (P<0.0001). Also, the second group had a higher mean fracture strength than the third group, but the difference was not significant (P=0.44) [2]. The results showed that the first group had significantly higher fracture strength than the other groups, consistent with the present study. In addition, the higher mean fracture strength of the second group compared to the third group confirmed the results of the present study. The only difference between the above and present studies is related to the non-significance of the difference in the fracture strength of the second and third groups. The possible cause is evaluating the fracture strength in the maxillary central incisors, while the present study was conducted on mandibular first molars.
In a study by Saboury et al. (2018), 30 implant-supported veneered zirconia crowns were evaluated on molar teeth. Samples (Copran Zri, WhitePeaks Dental Solutions GmbH Essen, Germany) were divided into three groups, including groups 1 without an occlusal hole, group 2 with an initial occlusal hole, and group 3 with an occlusal hole with zirconia wall around the hole. The results showed that preparing the occlusal channel reduced the fracture strength of the samples significantly (P<0.0001) [1]. In this study, the highest fracture strength was recorded in group 1. The results of this study are consistent with the present study.
CONCLUSION
The results of the present study showed that using an initial access channel with a diameter of 2.3 mm is the best choice to increase the fracture strength of hybrid implant-supported posterior monolithic zirconia crowns. However, when clinicians have to prepare an occlusal access hole with a bur, they should remember that increasing the diameter of the channel will significantly affect the crown’s strength.
SUGGESTIONS FOR FUTURE RESEARCH
The authors of this study suggest investigating the effect of cyclic fatigue on the fracture strength of implant-supported monolithic zirconia crowns in future studies.
ETHICAL STATEMENT
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences, Iran (approval no: IR.TBZMED.VCR.REC.1400.523).
AVAILABILITY OF DATA AND MATERIALS
The data used to support the findings of this study were supplied by the corresponding author [Y.A] under license and data will be available on request.
FUNDING
This study has been funded by the vice-chancellor for research (VCR) of Tabriz University of Medical Sciences (65626).
ACKNOWLEDGEMENTS
Declared none.


