Compound Odontoma in Canine Region and its Radiological Evidence: Case Reports
Abstract
Background:
Compound odontoma (CpOD) develops tooth germ-like structures but often lacks complete differentiation. Some authors recognize the compound odontoma as supernumerary teeth.
Objective:
This study aimed to present the analysis of orthodontic problems and radiological findings in three clinical cases of patients with complex odontoma.
Case Presentation:
The present three clinical cases of patients (two females and a male), aged from 14 to 25 years, had compound odontoma, which was confirmed through their radiological findings. Patients did not report symptoms associated with pain and discomfort in the area or genetic predisposition in the family. Orthodontists examined each clinical case with its individual problems and solutions. The findings were localized in the canine region, in 2 of the cases in the upper jaw and one in the lower. Only one patient with localization of the problem in the lower jaw had no disturbance in the eruption of the teeth in the affected dental arch, while in two patients with localization of the problem in the upper jaw, retention of permanent canines was found. In all three cases of the odontoma, there was one tooth with the reverse direction of the crown root. In one case, a supernumerary tooth near the odontoma was also observed. In all of the presented cases involving compound odontoma, there was one main well-formed and developed tooth, around which the other tooth-like structures were located, usually with a conical shape.
Conclusion:
CBCT contributes to establishing an accurate and detailed morphological characterization of the fundamental structures (teeth) in the odontoma.
1. INTRODUCTION
The hamartoma is a local malformation of the aberrant cells that resembles a neoplasm but is usually due to an overgrowth of normal mature cells and tissues that are local at their anatomical location. The term hamartoma derives from the Greek word “hamartia”, referring to a defect or error [1]. It is most often shaped as a disorganized type (not encapsulated and with irregular borders), with a predominance of one of the constituents [1]. Hamartomas occur in many different parts of the body, and in the area of the alveolar bone, it is of odontogenic origin and is called an odontoma. Therefore, an odontoma is a type of hamartoma lesion composed of tooth-like, not well-defined structures.
Odontomas are divided into the following types according to the morphology, characteristics, and organization of the dental mass of which they are composed: complex odontoma, compound odontoma, and mixed odontoma.
The complex odontoma (CxOD) is formed mainly by a solid tooth structure lacking pattern and shape. It is more common in the distal segments of both jaws. Some researchers believe that there is no sex dimorphism in the expression of this anomaly [2, 3], while others report a more common occurrence in women [4]. It has been reported that the complex odontoma can rarely erupt because it lacks periodontal ligaments. Its appearance in the oral cavity is a consequence of bone sequestration from its growth [5].
The compound odontoma (CpOD) contains enamel, dentin, cementum, and pulp, similar to normal teeth but with different morphology [6]. The odontoma, especially compound odontoma, develops structures, such as tooth germs, but often does not have complete differentiation of preameloblasts and ameloblasts, resulting in abnormal mineralization of the enamel organ [7].
Some researchers consider odontoma, particularly compound odontoma, as supernumerary teeth [8, 9], which is against its classification as a neoplasm with odontogenic origin.
In a retrospective study on 45 patients (15 CxOD and 30 CpOD), Kämmerer et al. found heterogeneous findings regarding the distribution in the lower jaw/upper jaw in a ratio of about 1: 0.55 (29/16) [10]. The compound odontoma was most often localized in the premaxilla (61%), and complex odontoma occurred in this region in 34% of the cases; this form was more localized in the distal parts of the jaws (59%) and rarely (only 7%) to the premolar area [11]. According to Boffano and Iatrou, over 45% of cases of odontoma are in the frontal segment of the jaws [12, 13]. According to Buchner, 75.9% of all odontogenic tumors are odontoma [14]. In a study on odontoma in Turkish patients, Avsever found that 36.4% were complex odontomas and 63.6% were compound odontomas; 18.2% of all cases were in the maxilla, and 81.8% in the mandible, and the most common location was the anterior mandibular region, where 40.9% of all cases were reported [15]. Pippi reported a frequency of odontoma of 0.64% among all patients and 30.4% among patients diagnosed with odontogenic tumors [16, 17]. The same author, who based his research on data from 42 peer-reviewed articles, reported that CxODs were more common in the maxillary incisors (165 cases) and mandibular molar region (247 cases), while CpODs were more often localized in the area of incisors and canines in both jaws.
The odontoma collections may have no clinical manifestation and may be detected by X-ray examination for another problem. According to various studies, 57% of patients develop clinical symptoms [16]. The most common manifestation is the impaction of permanent teeth, and the most affected are the upper incisors and canines, where most of the odontomas and, in particular, CpODs are localized. A less common symptom is a tumor lesion or an erupted part of the odontoma.
Radiologically, the two types of odontoma differ. CpODs are usually found between the teeth and consist of many tooth-like structures, which may include a supernumerary tooth. CxODs appear as a mass of dental tissues in an X-ray. It is possible that there is a lighter shadow around the odontoma collection due to debris or a preserved follicular sac, which is not always clearly defined.
2. CASE PRESENTATION
We present three clinical cases of patients with compound odontoma and an analysis of their radiological findings. Prior to their diagnosis and treatment, they completed an informed consent form for the use of their data for scientific purposes without disclosing their identities.
The aim is to analyze orthodontic problems and radiological findings in three clinical cases of patients with complex odontoma.
2.1. Clinical Case 1
We presented a case of a 25-year-old female who visited the orthodontic practice concerning impaired aesthetics and bad arrangement of teeth in the upper dental arch. The initial examination revealed deep and distal occlusion, retruded upper frontal teeth, and minimal spaces between the lower laterals and canines. We carried out X-ray examinations, OPG (orthopantomogram X-ray) and Ceph (cephalogram X-ray), for complete diagnosis (Fig. 1).
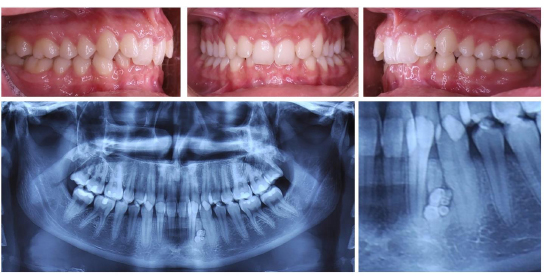
In a routine X-ray, an odontoma collection was observed in the area of the lower left lateral and canine. Exactly between the two roots, a structure with the characteristic of a tooth root was established, which raised suspicions of radix reliquiae from a primary canine. The image of the odontoma collection presented characteristics and localization typical for compound odontoma, i.e., radiological shadows with the characteristics of enamel, pulp, and germ sac. The X-ray image suggested resorption in the lower third of the canine root.
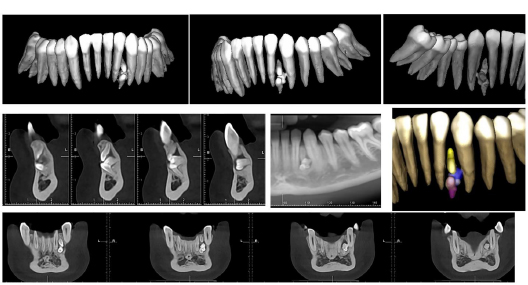
In order to obtain more information, a CBCT examination was performed (Fig. 2). The 3D examination revealed a compound odontoma composed of two interconnected tooth germs and one supernumerary conical tooth. This free-standing tooth was in situ in reverse, with a spike-shaped crown and incomplete root development. Its unusual direction was the reason to suspect radix relics in this area.
The other tooth-like structures were in the shape of a premolar, and the direction of the crown was vestibular. This was projected in the panoramic image as two or three small tooth germs. Another tooth included in the collection was a tooth-shaped germ with a crown protruding from the compact. These tooth-like structures were located in a common embryonic sac, giving the halo around the contrasting odontoma. A severe thinning of the vestibular compact in this area was assessed from the CBCT.
Surgical removal and curettage of the odontoma collection and orthodontic treatment after the recovery period were recommended to the patient. The CBCT images clarified the number and exact position of the parts of the compound odontoma, which were important for surgery planning.
After the surgical consultation, the severity and negatives of manipulation with vestibular access to the collection were explained to the patient. The proximity of the structures to the roots of the adjacent teeth and the traumatic nature of the procedure are risks that must be considered by the surgeon and the patient. The patient chose not to operate the odontoma and to be monitored periodically by X-rays.
2.2. Clinical Case 2
This was a clinical case of a 14-year-old male with complaints of a delayed eruption of the upper right canine (Fig. 3). The primary canine persisted in the mouth. The space in the maxillary dental arch was enough for the canine to erupt, and the occlusal relationships were not disturbed; class I with normal vertical coverage and coincidence of the midlines was observed. A bone swelling was palpated in the area above the primary canine, probably from the permanent canine. An OPG was performed, from which images of the upper right permanent canine and three supernumerary teeth were taken; one that was positioned parallel to the canine, one that was perpendicular to the axis of the primary canine, and one that was pointing in the direction of the crown of the canine. A CBCT scan was also taken (Fig. 4).

The CBCT examination revealed a supernumerary tooth, conical in shape, located palatal between the two premolars and an odontoma collection in the canine area. The dental germs in the compound odontoma were 4, located in a common follicular capsule covering their crowns. The crowns of the four dental germs were situated palatally and at the level of the coronal part of the permanent right canine, and their bodies were positioned as follows: two of them, each above the other perpendicular to the root of the lateral, one with a root passing between the canine and the first premolar and apex directed vestibular, and the last spike-shaped tooth from the collection had its root set palatal.
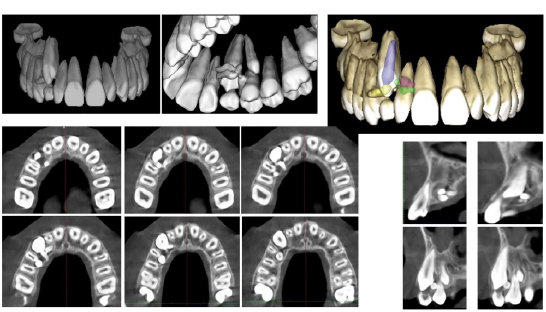
This odontoma formation led to the impaction of the canine, although it has a correct position and enough places in the dental arch. The OPG data led us to a hyperdontia diagnosis, while the CBCT image clarified that it was hyperdontia in the premolar area and compound odontoma in the canine area.
The data from the CBCT helped us make a differential diagnosis between supernumerary teeth and compound odontoma in the canine segment and also provided guidance for surgical intervention. After the removal of excess premolar and odontoma collection, we observed a spontaneous eruption of the canine.
The surgical stage preceded the start of the orthodontic treatment. Furthermore, sufficient space in the dental arch did not complicate or create additional risks of surgical manipulation. Young age and available eruptive biological forces compensated for the delay in the eruption of the upper right canine. The patient underwent conventional orthodontic treatment with the aim of leveling both dental arches (Fig. 5).

2.3. Clinical Case 3
The third case was of a 16-year-old female who attended our orthodontic practice for diastema and protruded maxillary frontal teeth. The initial examination revealed distal occlusion, narrowed upper jaw, protruding upper frontal teeth with diastema, and a short, low-attached labial frenulum (Fig. 6).

It is unusual for the upper left primary canine to be present at this age, suggesting impaction of the permanent canine. The examination revealed a change in the morphology of the hard palate in the canine area; it was compacted and overgrown. This suggests that the retained canine might be located in this area. A direct CBCT was performed in order to establish the topography and morphology of the impacted canine (Fig. 7).
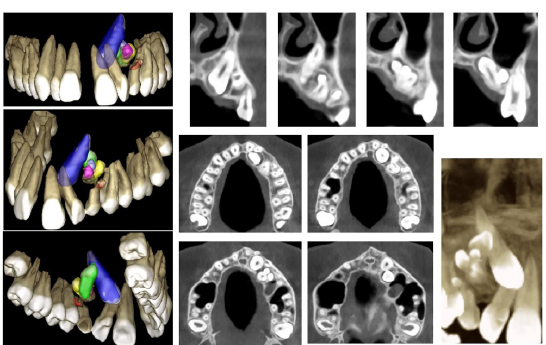
The three-dimensional examination revealed the impaction of the maxillary left canine and a large odontoma collection in the canine area. The impacted canine was positioned palatally and tangentially to the apical third of the lateral root, which altered its inclination. The crown was wrapped by the preserved follicular sac. Right in the canine area, but more palatal, there was an odontoma collection with characteristics of compound odontoma.
It consisted of a tooth in the shape of a canine, located central, with an inverted direction of the crown/root and 4-5 spike-shaped, well-formed, with all structures of tooth germs, surrounded by a common embryonic sac and one with a reduced size and a conical-shaped tooth germ outside it. This tooth-like configuration is the mechanical obstacle to canine eruption. The patient did not report any symptoms in the region, and the finding was made at this first visit to an orthodontist. Surgical removal of such a tooth-like structure requires a period of bone restoration before orthodontic traction of the canine to its place in the dental arch is planned. Therefore, orthodontic treatment of the problem, which is the motive for treating the patient, is the second stage after the surgical problem.
In this clinical case, the surgeon recommended that the surgical manipulations be done in two stages: first stage, extraction of the upper left temporary canine and leveling of the upper dental arch in order to reposition the upper incisors and open space in the area of tooth 23; second stage, extirpation of the odontoma collection and exposure of the retained canine. After the extraction of temporary tooth 63, the orthodontic leveling was carried out in the upper dental arch; the diastema was closed and prepared for surgical manipulation. In the second stage, the odontoma collection was removed, and the upper left canine was exposed palatally. Orthodontic treatment was carried out, tooth 23 was inserted into the upper dental arch, its rotation was corrected, and the occlusal relationships were normalized (Fig. 8).

3. DISCUSSION
In the three presented cases of compound odontoma, the findings were localized in the canine zone, in 2 of the cases in the upper jaw and in one in the lower, which is in accordance with the literature [10, 12, 17]. Two of the patients were females, and one was male. In all three cases, the findings were discovered by chance during the first checkup and appointment of an X-ray examination.
Only one patient with localization of the problem in the lower jaw had no disturbance in the eruption of the teeth in the affected dental arch, while in two patients with localization of the problem in the upper jaw, retention of permanent canines was found. In one case (case 2), a supernumerary tooth near the odontoma collection was reported. In all of the cases involving compound odontoma, there was one main well-formed and developed tooth, around which the other tooth-like structures were located, usually with a conical shape.
In all three cases with the odontoma, there was one tooth with the reverse direction of the crown root. In none of the cases root resorption of adjacent teeth was reported. Patients did not report symptoms associated with pain and discomfort in the area or genetic predisposition in the family. In both patients, in the maxillary region, the findings were situated palatally in the canine area, where a thickening was observed. Such thickening of the palatal surface may be observed in canine retention. However, in these cases, canines were located in other areas. In the patient with a finding in the mandible, the CBCT study helped to identify the contact of the compound odontoma to the cortical bone and the degree of its thinning.
The boundaries of the lesions and the position of the adjacent tooth roots were established. Pippi also recommends diagnosing the problem with CBCT to clarify the boundary of the collection and the thinning of the cortical bone or its perforation [17-19]. CBCT achieves an accurate and detailed morphological characterization of the fundamental structures (teeth) included in the odontoma [20, 21]. CBCT scanning offers volumetric images and assists in determining the position of the odontoma collection not only vertically but also in the vestibular-oral direction. For instance, in patient 2, the panoramic image provided information that led to the suspicion of three separate supernumerary teeth, while in reality, only one supernumerary tooth and compound odontoma were actually present.
Through CBCT scanning, a detailed assessment is made not only of the odontoma but also of the impacted teeth in terms of topography, the condition of the adjacent cortical bone, and the likelihood of root resorption. CBCT enables the planning of orthodontic treatment and the identification of the exact location for precise surgical excision.
Different treatment strategies were used in the three cases, which were in accordance with the individual characteristics of the orthodontic and surgical treatment strategies. In the first clinical case, the choice was to observe a possible change in the development and localization of the odontoma collection and, if necessary, surgical intervention. This approach is an informed choice of the patient and appropriate to the mature age and the absence of an orthodontic problem in the dentition. In the second and third cases, treatments were carried out, but their stages differed. In the second case, the topography of the odontoma collection and the favorable access to it made it possible to complete the surgical manipulation before the orthodontic treatment itself. In the third case, the first stage of the orthodontic treatment created conditions for a less risky surgical extirpation of the odontoma collection.
CONCLUSION
Early diagnosis of odontoma leads to less complicated treatment and a better prognosis. Quite often, odontoma is the cause of tooth impaction. Taking into account that the most common localization of compound odontoma is the incisor canine region, and canines are the teeth that are most often impacted, it is advisable to consider the possibility of an odontoma collection nearby when diagnosing canine retention. The CBCT diagnosis in cases involving compound odontoma enables differentiation from supernumerary teeth, identification of bone changes (resorption of the cortical wall or tooth roots), and exact planning of the orthodontic and surgical treatment.
LIST OF ABBREVIATIONS
| CBCT | = Cone Beam Computed Tomography |
| CpOD | = Compound odontoma |
| CxOD | = Complex odontoma |
| Ceph | = Cephalogram X-ray |
| OPG | = Orthopantomogram X-ray |
AVAILABILITY OF DATA AND MATERIALS
All the data and supporting information are provided within the article.
ACKNOWLEDGEMENTS
Declared none.


