All published articles of this journal are available on ScienceDirect.
Management of Impacted Mandibular Second Molar: A Case Report
Abstract
Introduction:
In rare cases, impacted second molars may create additional problems for orthodontic treatment. Both parents and the orthodontist should be aware of this problem early to prevent further complications. Good teamwork between the orthodontist and oral maxillofacial surgeon is needed in handling these cases, especially if it involves removing the impacted second molar. The right time to treat an impacted second molar is between the age of 11 to 14 years old. An impacted second molar can lead to a lack of arch length in the patient.
Objective:
The case report described the management of a female patient with a treated left-and-right impacted second molar in the mandible. The chief complaint of the patient was a protrusive mouth and having two impacted second molars, as told by her general dentist.
Case Report:
A 15-years-old female patient with Class I molar relationship, bilateral second molar impaction, and bimaxillary protrusion visited the clinic for orthodontic treatment. Extraction of four first premolar and mandibular second molar was completed. Both mandibular third molars were moved anteriorly to help close the space.
Conclusion:
Good cooperation from various disciplines and treatment planning to resolve the case can produce excellent and ideal results.
1. INTRODUCTION
The incidence of the third molar impaction rate is around 24.4%, whereas the mandibular second molar impaction rate is 0.03% [1-5]. Unilateral impaction of the mandibular second molar is more common than bilateral impaction. Such impaction occurs more frequently in the mandible than in the maxilla, and the impacted second molars are often mesially inclined. Several reasons for second molar impaction are inadequate arch length, the ectopic position of the tooth’s follicle, failure of the eruption mechanism, and an obstacle in the eruption path [1-5]. Most impacted second molars are mesially inclined and could be corrected using orthodontic mechanics [6].
The treatment options for an impacted second molar from the most conservative are (1) Tooth movement using orthodontic mechanics, (2) Surgical repositioning, (3) Tooth transplantation, and (4) Extraction of the impacted tooth. The success rate of correcting impacted second molar using orthodontic treatment is around 70% [5]. Correction of the impacted second molar using orthodontics is ideal during early adolescence when second molar root formation is still incomplete, and the mandibular third molars are not fully developed. Untreated impacted second molar could cause further problems such as anterior crowding, caries, root resorption, periodontitis of the adjacent molars, cysts, malocclusion, peri-coronal inflammation, and pain [4, 5, 7].
2. TREATMENT OBJECTIVE
This case report aims to describe the management of a patient with mandibular left and right impacted second molar treated in our clinic. Successful treatment requires a precise team and treatment plan that includes the general practitioner, orthodontist, periodontist, and oral surgeon.
3. CASE REPORT
A 15-year-old female patient came to the office with the chief complaint of “I have crooked teeth and difficulty eating.” Difficulty eating is most likely caused by the impacted second molar. The patient has had previous orthodontic treatment with other orthodontists. The patient was not taking any medicine and had no known drug allergies. Anamnesis showed a genetic predisposition run in the family, with her twin sister having the same type of problem.
Extraoral examination revealed that the patient has a bimaxillary protrusion with a convex profile. Intraoral examination revealed that the patient has all permanent dentitions except her third molar. The molar and canine relationship on both sides were Class I. The patient with an overbite and overjet was ideal (Fig. 1).
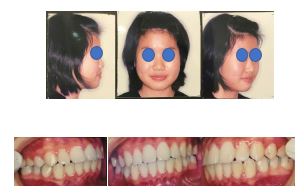
Cephalometric analysis indicated a Class I malocclusion with bimaxillary anterior protrusion (Fig. 2). The panoramic radiograph showed that the mandibular right and left second molar impacted with the mandibular right and left second molar impacted with the right and left third molar on top of the mandibular second molar. Mandibular first molar right and left tilted distally (Fig. 3).
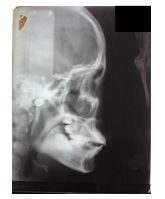

Treatment options were given to the patient and parents, along with the pros and cons of each treatment. Informed consent was signed. The treatment plan chosen by the patient and parents were: (1) Extract four 1st premolar (14 24 34 44) to relieve the bimaxillary protrusion (2) Extract mandibular right and left second molar (37 47) without damaging the alveolar bone and (3) Mesialize both mandibular 3rd molar (38 48) to close the space (Figs. 4 and 5).


Finding the correct oral and maxillofacial surgeon is very important, and communicating expectations before treatment are crucial to prevent misunderstanding. Emphasis on preserving the alveolar bone was discussed, and treatment could be completed. During the span of the orthodontic treatment, two teeth (16 36) needed to be treated endodontically by an endodontist (Fig. 5).
Treatment was completed, and both mandibular third molars were able to be mesialize successfully. From the panoramic radiograph (Fig. 5), the roots of the teeth were fairly parallel.
4. DISCUSSION
The patient comes to the clinic with the chief complaint of misaligned teeth (relapse). The patient reported that she had prior orthodontic treatment. Clinical and radiographic evaluation showed that the patient has a bimaxillary protrusion, and her mandibular left and right second molars (37 47) were still impacted with the third molars above them. After consultation with the patient and parents, along with educating them in regard to the finding, it was decided that there would be extraction of the four 1st premolars to relieve the bimaxillary protrusion and extraction of the mandibular left and right impacted second molars and advancing the wisdom teeth mesial to close the space orthodontically. The main advantage of doing space closure orthodontically is that the whole treatment will be finished post-orthodontic treatment without needing additional treatment, such as permanent restoration, which will also save treatment cost and time.
The biggest concern is during the extraction of the impacted molars. Preserving alveolar bone is important, especially since the third molar is mesial. After discussing with several oral and maxillofacial surgeons, an oral surgeon was willing to remove the impacted second molar and promised to minimize the damage to the alveolar bone. Adults can have less bone apposition when moving third molars into the narrowed space of second molars extraction sites, greater likelihood of loss of alveolar bone crest height on the mesial of the second molar roots, and in some patients, gingival recessions and root resorption could be seen [8-11]. Efficient orthodontic mechanics must be used to ensure the delivery of light forces and increase the interval between activations so that the soft tissues involved have time to recover and avoid the development of soft-tissue clefts, which tend to reopen spaces [9, 12, 13].
Impaction of the second molar is usually a problem of arch length deficiency. Most impaction of second molar occurs in more than one quadrant, which is much more common in the mandible than the maxilla. More commonly, an impacted third molar bud might compete for a position, which leads to impaction. The patient should be evaluated if the second molar has not erupted at its normal time, especially if the other teeth have erupted. An impending problem can be recognized from the physical examination, radiographic survey, projected space estimate, jaw growth patterns, and tooth position [14-16].
Fixed orthodontic treatment was started at the age of 15 and was done for 24 months. A good Class I intercuspation was achieved with a normal overbite and overjet (Figs. 4 and 5).
CONCLUSION
Impacted teeth need to be handled carefully. This article has shown good cooperation from various disciplines in dealing with impacted second molars that are extracted, which can produce excellent and ideal results. Successful treatment may require a teamwork approach that includes the general practitioner, orthodontist, periodontist, and oral surgeon. The patient and the family also needed to be educated to prevent any miscommunication and misunderstanding, especially with the difficulty of the procedures.
AUTHORS’ CONTRIBUTIONS
HH contributed to treating the case and providing the treatment photos and radiographs. HH initiated the case report and gave the final approval of the manuscript. IAH contributed to the literature review, completion, critical review, and manuscript revision.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient.
STANDARDS OF REPORTING
CARE guideline has been followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


